The Anatomy Involved: Understanding the Celiac Artery and the Median Arcuate Ligament.
In the field of human anatomy, understanding the intricate network of blood vessels is crucial. One such vessel that plays a vital role in supplying oxygenated blood to vital organs in the abdominal region is the celiac artery. This major branch of the abdominal aorta is involved in the supply of blood to several important structures including the stomach, liver, spleen, and pancreas.
The celiac artery, also known as the celiac trunk, originates just below the diaphragm. It is divided into three main branches – the left gastric artery, the splenic artery, and the common hepatic artery. These branches further divide into smaller vessels to ensure proper blood supply to specific areas of the abdomen.
However, the celiac artery is not free from the presence of surrounding structures that can impact its function. One such structure is the median arcuate ligament. This fibrous band lies above the celiac artery, forming an arch-like structure. The median arcuate ligament can sometimes exert pressure on the celiac artery, leading to a condition called median arcuate ligament syndrome.
Understanding the anatomy involved in the celiac artery and the median arcuate ligament is essential in diagnosing and treating potential complications. By studying the intricate network of blood vessels and the effect of adjacent structures, medical professionals can ensure the proper functioning of the celiac artery and the overall health of the abdominal region.
The Celiac Artery: Anatomy and Function
The understanding of the celiac artery and its function is crucial in comprehending the role it plays in the human body. The celiac artery is a major blood vessel that supplies oxygenated blood to various organs in the abdominal region. It is also involved in the supply of essential nutrients to these organs.
The celiac artery arises from the abdominal aorta, just below the diaphragm, and is located between the median arcuate ligament and the celiac plexus. This artery gives rise to three main branches: the left gastric artery, the splenic artery, and the common hepatic artery.
The left gastric artery supplies blood to the lesser curvature of the stomach and the lower esophagus. The splenic artery, as the name suggests, supplies blood to the spleen, pancreas, and parts of the stomach. The common hepatic artery, on the other hand, provides blood supply to the liver and gallbladder.
The function of the celiac artery is to ensure adequate blood supply to these abdominal organs, enabling them to function optimally. The oxygen-rich blood that it carries helps in the metabolic processes of the organs, ensuring their proper functioning.
Understanding the anatomy and function of the celiac artery is crucial in the diagnosis and treatment of conditions affecting the abdominal region. Any disruption in the blood flow through this artery can lead to various health issues, such as ischemia or organ malfunction.
In conclusion, the celiac artery is a vital blood vessel involved in supplying oxygenated blood and essential nutrients to the organs of the abdominal region. The proper understanding of its anatomy and function is essential in maintaining the overall health and well-being of an individual.
Origins and Course of the Celiac Artery
The celiac artery, also known as the celiac trunk, is a major blood vessel involved in the supply of blood to the abdominal organs. Understanding the origins and course of the celiac artery is essential in comprehending its role in the anatomy.
The celiac artery originates directly from the abdominal aorta, slightly below the diaphragm. It typically arises at the level of the upper border of the first lumbar vertebra. Its location makes it easily accessible and allows for efficient blood distribution to the organs in the abdominal cavity.
The celiac artery emerges as a single trunk and immediately divides into three main branches: the left gastric artery, the splenic artery, and the common hepatic artery. These branches supply blood to the stomach, spleen, and liver, respectively. The celiac artery is responsible for delivering oxygenated blood to these vital organs, which plays a crucial role in their proper functioning.
The course of the celiac artery continues as these three main branches travel in different directions to reach their respective target organs. The left gastric artery runs superiorly along the lesser curvature of the stomach, while the splenic artery courses posteriorly towards the spleen. The common hepatic artery takes a more complex path by giving off additional branches, such as the proper hepatic artery and the gastroduodenal artery, before reaching the liver.
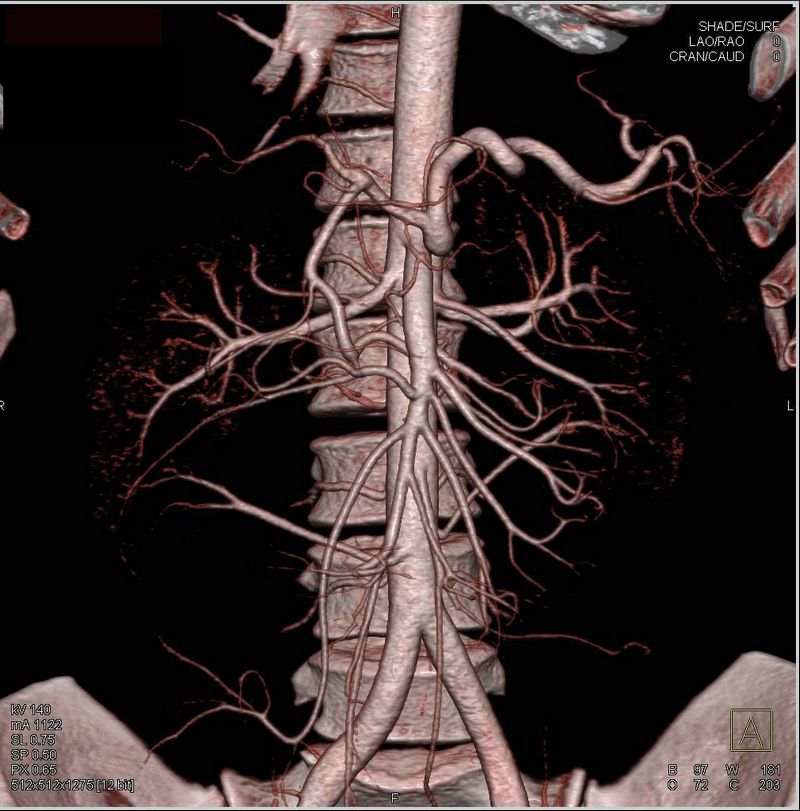
To better understand the course of the celiac artery and its branches, it is helpful to visualize their paths using anatomical diagrams. These diagrams illustrate the complexity and intricacy of the blood supply to the abdominal organs and highlight the interconnections between the celiac artery, the median arcuate ligament, and other blood vessels in the region.
In conclusion, the origins and course of the celiac artery are vital aspects of understanding its role in the anatomy. By knowing where the celiac artery arises from and how it distributes blood to the stomach, spleen, and liver, one can appreciate the significance of this blood vessel in maintaining proper organ function.
Branches of the Celiac Artery
The celiac artery, also known as the celiac trunk, is a major branch of the abdominal aorta. It is involved in supplying essential nutrients and oxygen to various organs and tissues in the upper abdomen. Understanding the branches of the celiac artery is crucial in comprehending the overall anatomy of the abdominal region.
The celiac artery gives rise to three main branches: the left gastric artery, the splenic artery, and the common hepatic artery. These branches further divide into smaller arteries, ensuring the efficient supply of blood to different structures.
-
Left Gastric Artery: This branch is responsible for supplying blood to the lesser curvature of the stomach. It also plays a role in forming the esophageal arterial network, which connects with the esophageal branches of other arteries.
-
Splenic Artery: The splenic artery is involved in nourishing the spleen, an important organ responsible for filtering blood and supporting the immune system. Additionally, it gives off several branches that supply the pancreas and parts of the stomach.
-
Common Hepatic Artery: The common hepatic artery supplies blood to the liver, an organ vital for metabolism and detoxification. This artery further divides into the proper hepatic artery and the gastroduodenal artery.
-
Proper Hepatic Artery: This branch provides blood to the liver and gives off several smaller arteries that supply different segments of the liver.
-
Gastroduodenal Artery: The gastroduodenal artery supplies blood to the stomach and the duodenum, the first part of the small intestine. It also gives off the right gastroepiploic artery, which supplies the greater curvature of the stomach, and the superior pancreaticoduodenal artery, which nourishes parts of the pancreas and the duodenum.
-
Understanding the branches of the celiac artery provides important insights into the blood supply network of the upper abdomen. This knowledge is crucial in diagnosing and treating various conditions that may affect these arteries and organs.
The Role of the Celiac Artery in Digestion
The celiac artery, also known as the celiac trunk, is a major branch of the abdominal aorta. It is responsible for supplying oxygenated blood to the abdominal organs involved in digestion, including the stomach, liver, spleen, and parts of the small and large intestine.
The celiac artery plays a vital role in the digestion process by ensuring that these organs receive the necessary nutrients and oxygen to function properly. It delivers oxygenated blood rich in nutrients, vitamins, and minerals after it has been processed by the liver.
The median arcuate ligament, a fibrous band of tissue, crosses over the celiac artery. This ligament can sometimes compress the celiac artery, leading to a condition known as median arcuate ligament syndrome (MALS). MALS can cause abdominal pain and digestive issues due to reduced blood flow to the affected organs. However, this condition is relatively rare.
The celiac artery branches into several smaller arteries that supply blood to specific regions of the digestive system. These branches include the left gastric artery, splenic artery, and common hepatic artery. The left gastric artery provides blood to the lesser curvature of the stomach, while the splenic artery supplies the spleen and parts of the stomach and pancreas. The common hepatic artery splits into the proper hepatic artery and the gastroduodenal artery, which supply the liver, gallbladder, and parts of the stomach and small intestine.
In addition to supplying blood to the digestive organs, the celiac artery also plays a role in regulating blood flow. It responds to changes in blood pressure and releases hormones that help control blood vessel diameter, influencing blood flow and blood pressure. This helps ensure that the digestive organs receive an adequate blood supply, especially during digestion when blood flow to these organs increases to aid in nutrient absorption.
In summary, the celiac artery is a crucial component of the digestive system. It supplies oxygenated blood to the abdominal organs involved in digestion and helps regulate blood flow to ensure proper organ function. Understanding the role of the celiac artery and its relationship with the median arcuate ligament can provide valuable insights into the anatomy and physiology of digestion.
Common Disorders Affecting the Celiac Artery
The celiac artery is a major blood vessel that plays a crucial role in supplying oxygenated blood to the abdominal organs. It arises from the aorta and branches off into three main arteries: the left gastric artery, the splenic artery, and the common hepatic artery. However, various disorders can affect the celiac artery, causing significant health problems for individuals.
1. Celiac Artery Stenosis: This condition occurs when there is a narrowing of the celiac artery, reducing blood flow to the abdominal organs. It can be caused by atherosclerosis, where plaques build up inside the artery walls, or by the compression of the median arcuate ligament. Celiac artery stenosis can lead to abdominal pain, weight loss, and an increased risk of developing mesenteric ischemia.
2. Celiac Artery Aneurysm: A celiac artery aneurysm is a bulging or ballooning of the artery wall. It can be caused by underlying connective tissue disorders, such as Ehlers-Danlos syndrome, or by atherosclerosis. Celiac artery aneurysms are relatively rare, but if left untreated, they can rupture and cause life-threatening internal bleeding.
3. Median Arcuate Ligament Syndrome: The median arcuate ligament is a fibrous band of tissue that crosses over the celiac artery. In some individuals, this ligament can compress and constrict the celiac artery, leading to symptoms such as abdominal pain, digestive issues, and weight loss. This condition is more common in women and may be exacerbated by stress or physical activity.
4. Celiac Artery Thrombosis: Celiac artery thrombosis occurs when a blood clot forms inside the artery, blocking blood flow to the abdominal organs. It can result from various underlying conditions, such as hypercoagulable disorders, vasculitis, or trauma. Celiac artery thrombosis is a severe condition that requires immediate medical intervention to prevent organ damage or necrosis.
5. Celiac Artery Dissection: Celiac artery dissection is a rare condition where a tear occurs in the inner layer of the artery wall, causing blood to flow between the layers. This can lead to a reduction in blood flow to the abdominal organs and potentially result in organ ischemia. The exact cause of celiac artery dissection is unknown, but it is believed to be associated with underlying connective tissue disorders or trauma.
In conclusion, understanding the common disorders that affect the celiac artery is crucial for early detection and appropriate management. If you experience persistent abdominal pain or other concerning symptoms, it is important to consult a healthcare professional for further evaluation and guidance.
The Median Arcuate Ligament: Structure and Implications
The median arcuate ligament is an important anatomical structure found in the abdomen, specifically in relation to the celiac artery. Understanding the structure and implications of this ligament is crucial in grasping the overall anatomy and function of the celiac artery.
The median arcuate ligament is a fibrous band of tissue that spans across the anterior aspect of the aorta, just below the diaphragm. It connects the right and left crura of the diaphragm and creates a tunnel-like space through which the celiac artery passes.
Being positioned in such a way, the median arcuate ligament can have implications on the blood flow to the celiac artery. In some individuals, the ligament may become tight or constrictive, leading to a condition called median arcuate ligament syndrome (MALS).
In cases of MALS, the tight median arcuate ligament can compress and narrow the celiac artery, resulting in reduced blood flow to the abdominal organs. This can cause symptoms such as abdominal pain, digestive issues, and weight loss.
Diagnosis of MALS typically involves imaging studies such as ultrasound, CT scan, or magnetic resonance angiography. Treatment options may include medications for symptom management, lifestyle modifications, or surgical intervention to release the constriction of the ligament.
Understanding the structure and implications of the median arcuate ligament is crucial in the diagnosis and management of celiac artery-related conditions. It allows healthcare professionals to accurately assess the potential impact of the ligament on blood flow and to develop appropriate treatment plans for affected individuals.
Location and Attachment of the Median Arcuate Ligament
The median arcuate ligament is a fibrous band that is part of the anatomy of the celiac artery. It is an important structure to understand in order to fully comprehend the complexities of the celiac artery’s anatomy.
The median arcuate ligament is located just below the diaphragm and is positioned in such a way that it forms an arch-like shape. It attaches to the front of the lumbar vertebrae, specifically the first and second lumbar vertebrae.
It is important to note that the median arcuate ligament can vary in its attachment points and its shape among individuals. In some cases, it may be completely absent. However, its presence and proper attachment play a crucial role in maintaining the normal function of the celiac artery.
- Understanding the attachment of the median arcuate ligament is essential because it can have significant implications for blood flow to the abdominal organs.
- If the ligament is too tight or misplaced, it may compress or constrict the celiac artery, leading to a condition known as median arcuate ligament syndrome.
- This syndrome can cause various symptoms such as abdominal pain, weight loss, and digestive issues because of reduced blood flow to the organs supplied by the celiac artery, including the liver, stomach, and spleen.
In conclusion, a thorough understanding of the location and attachment of the median arcuate ligament is crucial in comprehending the anatomy and function of the celiac artery. Knowing its role and potential implications can help in diagnosing and treating conditions related to the median arcuate ligament.
Role of the Median Arcuate Ligament in Abdominal Stability
The understanding of the anatomy involved in abdominal stability is essential for diagnosing and treating various abdominal conditions. One of the important structures to consider is the median arcuate ligament, which plays a significant role in maintaining the stability of the abdomen.
The median arcuate ligament is a fibrous band that connects the two sides of the diaphragm and forms a strong support for the celiac artery. It runs horizontally across the front of the aorta and can sometimes cause compression of the celiac artery, leading to a condition known as median arcuate ligament syndrome.
When the median arcuate ligament tightens or compresses the celiac artery, it can result in abdominal pain, especially after meals. This compression can also reduce blood flow to the digestive organs, leading to symptoms such as nausea, vomiting, and weight loss.
The role of the median arcuate ligament in abdominal stability is crucial because it helps maintain the position and function of the celiac artery. The celiac artery is responsible for supplying blood to important abdominal organs, including the liver, stomach, and spleen.
Without the proper functioning of the celiac artery, these organs may not receive enough oxygen and nutrients, leading to various health issues. The median arcuate ligament acts as a stabilizing force, preventing any excessive movement or displacement of the celiac artery, ensuring a continuous blood supply to the abdominal organs.
Understanding the role of the median arcuate ligament in abdominal stability is essential in diagnosing and managing conditions such as median arcuate ligament syndrome. By identifying any compression or tightness of the ligament, healthcare professionals can provide appropriate treatment options, including surgical intervention if necessary.
In conclusion, the median arcuate ligament plays a crucial role in maintaining abdominal stability by supporting the celiac artery. Its role in stabilizing the celiac artery ensures proper blood supply to vital abdominal organs. Understanding the anatomy and function of the median arcuate ligament is essential for diagnosing and managing abdominal conditions associated with its compression or tightness.
Disorders Associated with the Median Arcuate Ligament
The median arcuate ligament is a band of connective tissue that crosses over the celiac artery, a major branch of the abdominal aorta. While it plays an important role in supporting the celiac artery, the ligament can also be associated with certain disorders and conditions.
Celiac Artery Compression Syndrome:
The most common disorder associated with the median arcuate ligament is celiac artery compression syndrome, also known as median arcuate ligament syndrome. This condition occurs when the ligament compresses the celiac artery, resulting in reduced blood flow to the organs supplied by the artery.
Celiac artery compression syndrome can cause a range of symptoms, including abdominal pain after meals, weight loss, nausea, and vomiting. In severe cases, it can lead to malnutrition and organ damage.
Inflammatory Conditions:
Inflammation of the median arcuate ligament can also occur, leading to a condition known as median arcuate ligament syndrome. This can be caused by various factors, including infections, autoimmune disorders, or trauma.
When the ligament becomes inflamed, it can cause abdominal pain, tenderness, and difficulty eating. Treatment for this condition typically involves addressing the underlying cause of the inflammation and managing the symptoms.
Abnormalities:
The median arcuate ligament can also be subject to certain abnormalities that can contribute to disorders. For example, an abnormal attachment of the ligament to the diaphragm can cause compression of the celiac artery.
Other abnormalities, such as an elongated or hypertrophied ligament, can also result in compression of the celiac artery and lead to related symptoms.
Treatment:
Treatment for disorders associated with the median arcuate ligament may involve a combination of medical management and surgical intervention. Medications may be prescribed to manage symptoms such as pain and inflammation.
In cases where conservative treatment is ineffective, surgical options may be considered. These can include ligament release or angioplasty to improve blood flow to the affected organs.
Conclusion:
Understanding the disorders associated with the median arcuate ligament is important for diagnosing and managing related conditions. While these disorders can cause significant symptoms and complications, appropriate treatment can help improve outcomes for affected individuals.
Understanding the Relationship Between the Celiac Artery and the Median Arcuate Ligament
The anatomy of the celiac artery and the median arcuate ligament is an important area of study for understanding the blood flow and vascular supply to the abdominal organs. The celiac artery, also known as the celiac trunk, is a major branch of the abdominal aorta. It supplies blood to the stomach, liver, spleen, and other structures in the upper abdomen.
The celiac artery usually arises from the anterior aspect of the abdominal aorta just below the diaphragm. It then divides into three main branches: the left gastric artery, the splenic artery, and the common hepatic artery. These branches provide vital blood supply to the respective organs.
The median arcuate ligament is a fibrous band of tissue that stretches across the front of the abdominal aorta, just above the celiac artery. It forms an arch-like structure, hence the name “arcuate ligament.” This ligament is one of the components of the diaphragmatic crura, which help to support and stabilize the diaphragm.
In some individuals, the median arcuate ligament can cause compression or narrowing of the celiac artery, resulting in a condition called median arcuate ligament syndrome (MALS). MALS can lead to abdominal pain, digestive issues, and weight loss. It is more common in women and may be associated with abnormal vascular anatomy or fibrous bands around the celiac artery.
To diagnose MALS, various imaging techniques, such as CT angiography or magnetic resonance angiography, can be used to visualize the celiac artery and the median arcuate ligament. Treatment options for MALS include surgical release of the median arcuate ligament to alleviate the compression on the celiac artery.
In conclusion, understanding the relationship between the celiac artery and the median arcuate ligament is crucial for assessing and managing conditions such as median arcuate ligament syndrome. Proper knowledge of the anatomy and function of these structures helps in identifying potential vascular issues and formulating appropriate treatment plans.
Anatomy of the Celiac Artery and the Median Arcuate Ligament Connection
The celiac artery is an important blood vessel that supplies oxygenated blood to the organs of the upper abdomen. It is also known as the celiac trunk or the celiac axis. The celiac artery is involved in the supply of blood to the liver, stomach, spleen, and parts of the small and large intestines.
The celiac artery arises from the abdominal aorta, just below the diaphragm, at the level of the T12 vertebra. It is located behind the median arcuate ligament, which is a fibrous band of tissue that stretches across the front of the aorta. The median arcuate ligament is formed by the fusion of the right and left crura of the diaphragm.
The celiac artery typically gives rise to three branches, known as the left gastric artery, the splenic artery, and the common hepatic artery. The left gastric artery supplies blood to the lesser curvature of the stomach, while the splenic artery supplies blood to the spleen. The common hepatic artery further divides into the proper hepatic artery and the gastroduodenal artery, which supply blood to the liver, gallbladder, and parts of the stomach and small intestine, respectively.
The connection between the celiac artery and the median arcuate ligament is important because the ligament can sometimes compress the artery, leading to a condition known as median arcuate ligament syndrome. This condition can cause symptoms such as chronic abdominal pain, weight loss, and digestive issues. Treatment options for median arcuate ligament syndrome may include medication, angioplasty, or surgery to relieve the compression of the celiac artery.
In conclusion, understanding the anatomy of the celiac artery and the median arcuate ligament connection is crucial for diagnosing and treating conditions that involve these structures. The celiac artery is responsible for supplying blood to important organs in the upper abdomen, while the median arcuate ligament can sometimes cause compression of the artery, leading to symptoms and complications. Further research and clinical studies are needed to improve our understanding of this anatomical relationship and develop effective treatment strategies.
The Effect of the Median Arcuate Ligament on Celiac Artery Blood Flow
The celiac artery is one of the major blood vessels in the abdominal region. It supplies blood to several organs including the stomach, liver, and spleen. The understanding of its anatomy and the structures involved is crucial to ensure proper blood flow to these organs.
One of the key structures that plays a role in the celiac artery’s blood flow is the median arcuate ligament. This ligament is a fibrous band that crosses over the celiac artery, creating a compression effect. It is located at the level of the diaphragm, in the region where the aorta descends.
The median arcuate ligament can have a significant impact on the blood flow through the celiac artery. When it is tight or hypertrophic, it can cause compression of the artery, leading to reduced blood flow. This can result in various symptoms and conditions, including abdominal pain, nausea, and weight loss.
Understanding the anatomy and function of the median arcuate ligament is essential in diagnosing and treating conditions related to celiac artery blood flow. Imaging techniques such as ultrasound, CT scans, and angiography can help visualize the ligament and assess its effect on blood flow.
Treatment options for patients with celiac artery compression syndrome, caused by the median arcuate ligament, may include surgical interventions like ligament release or arterial bypass procedures. In some cases, a multidisciplinary approach involving vascular surgeons, radiologists, and gastroenterologists may be necessary.
| Weight loss | Diarrhea | Bloating |
In conclusion, the median arcuate ligament plays a significant role in the blood flow through the celiac artery. Understanding its anatomy and the impact it can have on the artery is crucial in diagnosing and treating conditions related to celiac artery blood flow. Proper evaluation and management by a healthcare team can help improve symptoms and ensure adequate blood supply to the organs supplied by the celiac artery.
Medical Conditions Linked to Celiac Artery Compression by the Median Arcuate Ligament
The understanding of the anatomy involved in the compression of the celiac artery by the median arcuate ligament has contributed to the identification of several medical conditions that can be linked to this phenomenon. The celiac artery is a major blood vessel that supplies oxygenated blood to the abdominal organs, including the liver, stomach, and spleen. It passes through an opening formed by the median arcuate ligament, which is a fibrous band that connects the two sides of the diaphragm.
When the median arcuate ligament becomes hypertrophic or tight, it can exert pressure on the celiac artery, leading to a condition known as celiac artery compression syndrome (CACS). CACS can result in a variety of symptoms and medical conditions, including:
- Abdominal Pain: CACS can cause chronic abdominal pain, which is typically located in the upper abdomen and may be worsened by eating. The pain is often described as dull or cramp-like.
- Weight Loss: CACS can lead to weight loss due to impaired blood flow to the abdominal organs, which can affect digestion and nutrient absorption.
- Nausea and Vomiting: These symptoms may occur as a result of the compromised blood supply to the stomach and intestines.
- Early Satiety: CACS can cause a feeling of fullness or satiety after eating small amounts of food. This can contribute to weight loss and malnutrition.
- Gastric Ulcers: The reduced blood flow to the stomach can lead to the development of gastric ulcers.
- Hepatic Ischemia: CACS can result in reduced blood flow to the liver, which may lead to liver dysfunction or damage.
- Intestinal Ischemia: In severe cases, CACS can cause ischemia or lack of blood supply to the intestines, which can be a life-threatening condition requiring immediate medical intervention.
It is important for healthcare professionals to be aware of the potential link between these medical conditions and celiac artery compression by the median arcuate ligament. Diagnosis of CACS can be challenging, as symptoms can be nonspecific and other conditions may need to be ruled out. Imaging studies, such as angiography or computed tomography angiography, may be used to visualize the anatomy and assess blood flow in the celiac artery.
| Abdominal Pain | Dull or cramp-like pain in the upper abdomen |
| Weight Loss | Unintentional weight loss |
| Nausea and Vomiting | Feeling nauseous and vomiting |
| Early Satiety | Feeling full or satisfied after eating small amounts |
| Gastric Ulcers | Development of ulcers in the stomach |
| Hepatic Ischemia | Liver dysfunction or damage |
| Intestinal Ischemia | Life-threatening lack of blood supply to the intestines |
Early recognition and appropriate management of CACS are essential to prevent complications and improve patient outcomes. Treatment options may include lifestyle modifications, medication to relieve symptoms, or in severe cases, surgical intervention to release the compression on the celiac artery.
Diagnostic Techniques for Celiac Artery and Median Arcuate Ligament Disorders
The diagnosis of disorders involving the celiac artery and median arcuate ligament of the diaphragm requires a combination of clinical evaluation, imaging techniques, and laboratory tests. Due to their proximity and interrelation, the evaluation of these structures often occurs simultaneously.
Clinical Evaluation:
- Patients presenting with symptoms such as epigastric pain, weight loss, nausea, and vomiting should undergo a thorough clinical evaluation to assess the possibility of celiac artery and median arcuate ligament disorders.
- A detailed medical history, physical examination, and review of symptoms provide valuable insights into potential underlying conditions.
Imaging Techniques:
- Ultrasound: This non-invasive imaging technique can provide initial information about the celiac artery, including blood flow and potential narrowing or occlusion. However, its effectiveness may vary depending on the operator’s expertise and patient characteristics.
- Computed Tomography (CT) Scan: CT scans offer detailed cross-sectional images of the celiac artery and surrounding structures. It can identify stenosis, calcifications, and anatomical variations. CT angiography may also be performed to visualize blood flow through the celiac artery.
- Magnetic Resonance Imaging (MRI): MRI is useful for further assessing the celiac artery and median arcuate ligament. It can provide high-resolution images without ionizing radiation. Magnetic resonance angiography (MRA) can be performed to visualize blood flow through the celiac artery.
- Angiography: In some cases, angiography may be required for a more definitive diagnosis. It involves the injection of contrast dye into the celiac artery to assess blood flow and detect any abnormalities.
Laboratory Tests:
- Blood Tests: A complete blood count (CBC) and metabolic panel can help assess overall health and identify any underlying conditions that may contribute to celiac artery and median arcuate ligament disorders.
- Doppler Ultrasonography: This technique uses sound waves to evaluate blood flow velocity and direction in the celiac artery. It can detect stenosis, occlusion, or other abnormalities.
Conclusion:
The diagnosis of celiac artery and median arcuate ligament disorders requires a multidisciplinary approach involving clinical evaluation, imaging techniques, and laboratory tests. Combining these diagnostic tools can help accurately identify and assess the extent of the conditions, enabling appropriate treatment planning.
Treatment Options for Celiac Artery and Median Arcuate Ligament Disorders
Understanding the anatomy and function of the celiac artery and the median arcuate ligament is crucial for identifying and treating disorders affecting these structures. Depending on the specific condition and severity, various treatment options may be considered.
1. Conservative Management:
In mild cases, where symptoms are not severe or do not significantly impact daily life, conservative management options may be recommended. This typically involves implementing lifestyle changes and dietary modifications to improve symptoms. Patients may be advised to avoid certain triggers or foods that exacerbate symptoms. In some cases, medications such as proton pump inhibitors or antacids may be prescribed to help control acid reflux or manage symptoms.
2. Surgical Intervention:
In more severe cases, surgical intervention may be necessary to address the underlying issues causing celiac artery or median arcuate ligament disorders. The type of surgical procedure will depend on the specific condition and its severity, as well as the individual patient’s overall health and medical history.
Common surgical procedures for treating celiac artery and median arcuate ligament disorders include:
- Celiac artery decompression: This procedure involves releasing the constriction of the celiac artery by dividing the median arcuate ligament. This can be done through open surgery or minimally invasive techniques, such as laparoscopy. By relieving the compression, blood flow to the celiac artery is restored, alleviating symptoms and improving overall function.
- Bypass surgery: In cases where the celiac artery is severely blocked or damaged, bypass surgery may be necessary. This involves creating a new pathway for blood to flow around the blocked or damaged portion of the artery, restoring blood flow to the organs supplied by the celiac artery.
- Angioplasty and stenting: For certain conditions, such as celiac artery stenosis, angioplasty and stenting may be performed. This minimally invasive procedure involves using a catheter to insert a balloon and stent into the narrowed or blocked area of the artery. The balloon is inflated to widen the artery and the stent is left in place to keep it open, allowing for improved blood flow.
3. Collaborative Care:
Depending on the specific disorder and its impact on the patient’s overall health and well-being, a multidisciplinary approach to treatment may be recommended. This may involve collaboration between various healthcare professionals, such as cardiovascular surgeons, gastroenterologists, dietitians, and pain management specialists. Together, they can develop a comprehensive treatment plan that addresses the patient’s specific needs and aims to improve overall quality of life.
It is important to consult with a healthcare professional to determine the most appropriate and effective treatment options for celiac artery and median arcuate ligament disorders. Each individual case is unique, and treatment plans should be tailored to meet the specific needs and goals of the patient.
Conservative Management Approaches
Understanding the anatomy of the median arcuate ligament and its involvement with the celiac artery is crucial in designing appropriate management approaches for patients suffering from related conditions. While surgical intervention may be necessary in some cases, conservative management approaches can also be effective in managing symptoms and improving the quality of life for patients.
Dietary Modifications:
- Avoiding foods that trigger symptoms can help in relieving abdominal pain, bloating, and diarrhea.
- A gluten-free diet is often recommended for patients with celiac disease, as it can reduce inflammation and heal the damage to the small intestine.
- Working with a registered dietitian can be helpful in developing an individualized dietary plan.
Medication:
- Antacids and acid reducers can help in reducing stomach acid production, alleviating symptoms such as heartburn and indigestion.
- Prokinetic medications can improve gastrointestinal motility and relieve symptoms like nausea and vomiting.
- Pain medications may be prescribed to manage abdominal pain.
Lifestyle Changes:
- Stress management techniques, such as yoga and meditation, can help in reducing stress-related symptoms.
- Regular exercise can improve overall health and digestion.
- Quitting smoking can have numerous benefits for general health and may help in managing symptoms.
Monitoring and Follow-up:
Patient education about their condition and regular follow-up appointments with healthcare providers are essential for monitoring symptoms, adjusting treatment plans, and addressing any concerns or complications that may arise.
Conclusion:
Conservative management approaches play an important role in the overall care of patients with median arcuate ligament syndrome and related conditions. These approaches aim to alleviate symptoms, improve the quality of life, and prevent the need for surgical interventions in some cases. However, it is important to note that the effectiveness of these approaches may vary depending on the individual, and healthcare providers should personalize the management plan based on each patient’s specific needs.
Surgical Interventions for Celiac Artery and Median Arcuate Ligament Disorders
Surgical intervention may be required for patients with disorders related to the celiac artery and the median arcuate ligament. These disorders can cause symptoms such as abdominal pain, weight loss, and digestive issues, and can have a significant impact on a patient’s quality of life. Understanding the anatomy and function of the celiac artery and the median arcuate ligament is crucial in determining the appropriate surgical approach.
The celiac artery is a major branch of the abdominal aorta that supplies oxygenated blood to the abdominal organs, including the stomach, liver, and spleen. The median arcuate ligament is a fibrous band that crosses over the celiac artery, forming the anterior wall of the celiac trunk. However, in some individuals, the ligament can compress the celiac artery, leading to conditions such as celiac artery compression syndrome or median arcuate ligament syndrome.
One surgical intervention for celiac artery compression syndrome is known as celiac artery decompression. During this procedure, the surgeon releases the constriction caused by the median arcuate ligament, allowing for improved blood flow to the abdominal organs. This can help alleviate symptoms and improve the patient’s overall health. The surgery may involve removing a portion of the median arcuate ligament or dividing it to relieve the pressure on the celiac artery.
In cases where the celiac artery is significantly damaged or blocked, a bypass surgery may be performed. This involves creating a new pathway for blood flow by using a graft to connect the aorta to one of the branches of the celiac artery. This bypass allows blood to bypass the damaged or blocked area and ensures that the abdominal organs continue to receive adequate blood supply.
Another surgical intervention for celiac artery and median arcuate ligament disorders is angioplasty. This procedure involves using a balloon-tipped catheter to widen the celiac artery and improve blood flow. In some cases, a stent may be placed to help keep the artery open. Angioplasty can be an effective minimally invasive option for patients who are not good candidates for open surgery.
In conclusion, surgical interventions for celiac artery and median arcuate ligament disorders play a crucial role in restoring proper blood flow to the abdominal organs and alleviating symptoms. Understanding the anatomy and function of these structures is essential in determining the most appropriate surgical approach for each individual case. With advancements in surgical techniques, patients can now benefit from less invasive procedures that offer faster recovery times and improved outcomes.
Outcome and Prognosis for Patients with Celiac Artery and Median Arcuate Ligament Disorders
Understanding the anatomy of the celiac artery and the median arcuate ligament is crucial when considering the outcome and prognosis for patients with disorders affecting these structures. The celiac artery is a major blood vessel that supplies blood to the abdominal organs including the liver, pancreas, and stomach. The median arcuate ligament is a fibrous band that crosses over the celiac artery, potentially causing compression and narrowing of the artery.
Patients with celiac artery and median arcuate ligament disorders can experience a variety of symptoms including abdominal pain, weight loss, and digestive issues. The severity of these symptoms can vary depending on the extent of arterial compression and the duration of the disorder.
Treatment options for patients with celiac artery and median arcuate ligament disorders may include conservative management, such as dietary modifications and medications to relieve symptoms. However, in more severe cases, surgical intervention may be necessary to alleviate arterial compression and restore blood flow.
The prognosis for patients with celiac artery and median arcuate ligament disorders can vary depending on several factors. Early diagnosis and treatment are key to improving outcomes, as delayed intervention may lead to more severe complications. The success of surgical intervention also plays a significant role in determining prognosis, with a higher success rate associated with complete resolution of symptoms and restoration of normal blood flow.
| Extent of Arterial Compression | The degree to which the celiac artery is compressed can impact the severity of symptoms and the potential for complications. |
| Duration of the Disorder | Patients with long-standing celiac artery and median arcuate ligament disorders may have a poorer prognosis compared to those with a more recent onset of symptoms. |
| Surgical Success | The success of surgical intervention in relieving arterial compression and restoring blood flow is a significant factor in determining prognosis. |
In conclusion, the outcome and prognosis for patients with celiac artery and median arcuate ligament disorders can vary depending on the extent of arterial compression, the duration of the disorder, and the success of surgical intervention. Early diagnosis and treatment are crucial for improving outcomes and preventing complications. Further research is needed to better understand the long-term prognosis for this patient population.
Question-answer:
What is the celiac artery?
The celiac artery is a major branch of the abdominal aorta that supplies blood to the abdominal organs, including the liver, stomach, spleen, and pancreas.
What is the median arcuate ligament?
The median arcuate ligament is a fibrous band that crosses over the celiac artery and the lumbar spine. It can sometimes cause compression of the celiac artery, leading to a condition called median arcuate ligament syndrome.
What are the symptoms of median arcuate ligament syndrome?
The symptoms of median arcuate ligament syndrome can vary, but common symptoms include chronic abdominal pain, especially after eating, weight loss, nausea, and vomiting.
How is median arcuate ligament syndrome diagnosed?
Median arcuate ligament syndrome can be diagnosed through various medical imaging tests, such as ultrasound, CT scan, or magnetic resonance angiography. These tests can help visualize the celiac artery and determine if there is any compression or narrowing caused by the median arcuate ligament.
What are the treatment options for median arcuate ligament syndrome?
Treatment options for median arcuate ligament syndrome may include lifestyle modifications, such as avoiding large meals or certain trigger foods, as well as medications to manage pain. In severe cases, surgical intervention may be needed to relieve the compression on the celiac artery.
What is the function of the celiac artery?
The celiac artery is responsible for supplying blood to the abdominal organs, including the liver, stomach, spleen, and pancreas.