 Understanding the Potential Consequences and Predictions for Mesenteric Thrombosis
Understanding the Potential Consequences and Predictions for Mesenteric Thrombosis
Mesenteric thrombosis is a serious condition that occurs when a blood clot forms in one of the arteries that supply blood to the intestines. This can lead to a blockage of blood flow and cause tissue damage or death in the affected area. The prognosis for mesenteric thrombosis depends on several factors, including the extent of the clot, the presence of underlying medical conditions, and the promptness of treatment.
One of the main outcomes of mesenteric thrombosis is ischemia, which occurs when the affected area does not receive enough blood and oxygen. This can result in severe abdominal pain, nausea, vomiting, and diarrhea. If left untreated, mesenteric thrombosis can lead to bowel infarction, a condition where the affected portion of the intestine dies. Bowel infarction is a life-threatening condition that requires emergency surgery to remove the dead tissue.
The prognosis for mesenteric thrombosis is generally poor, especially if the condition is not diagnosed and treated promptly. Without treatment, the mortality rate for mesenteric thrombosis is high, with some studies reporting rates as high as 50-90%. However, with early intervention, the prognosis can improve significantly. Treatment options for mesenteric thrombosis include anticoagulant therapy to dissolve the clot and surgery to remove the blockage or repair the damaged blood vessels.
It is important for individuals at risk of mesenteric thrombosis to be aware of the symptoms and seek medical attention immediately if they experience abdominal pain that is severe and persistent, especially if accompanied by other symptoms such as nausea and vomiting. Early diagnosis and treatment can greatly improve the outcome and prognosis for mesenteric thrombosis, reducing the risk of bowel infarction and death.
Mesenteric thrombosis is a serious condition with potentially dire consequences. The prognosis for mesenteric thrombosis depends on various factors, including the extent of the clot, the presence of underlying medical conditions, and the timeliness of treatment. Prompt medical attention is crucial for improving outcomes and reducing the risk of complications such as bowel infarction. Individuals at risk should be vigilant for symptoms and seek immediate medical attention if they suspect mesenteric thrombosis.
What happens if the superior mesenteric artery is blocked?
If the superior mesenteric artery becomes blocked, it can lead to a condition known as mesenteric thrombosis. This occurs when a blood clot forms in the artery, cutting off the blood supply to the intestines.
When the blood flow to the intestines is compromised, it can result in tissue damage and can be life-threatening if left untreated. The lack of blood supply can lead to ischemia, which is a condition where the tissues do not receive enough oxygen and nutrients.
Common symptoms of a blocked superior mesenteric artery include severe abdominal pain, nausea, vomiting, and diarrhea. These symptoms typically develop suddenly and can indicate a medical emergency.
If left untreated, mesenteric thrombosis can lead to complications such as bowel infarction, which is the death of intestinal tissue. This can result in a perforation or rupture of the intestines, leading to infection and potentially sepsis.
Early diagnosis and prompt treatment are crucial to improving outcomes for individuals with mesenteric thrombosis. Treatment options may include anticoagulant medications to dissolve the blood clot, surgical intervention to remove the clot, or bypass surgery to restore blood flow to the intestines.
Recovery and prognosis can vary depending on the severity of the blockage, the extent of tissue damage, and the individual’s overall health. In some cases, individuals may experience long-term complications such as chronic abdominal pain or malabsorption.
A blocked superior mesenteric artery can have serious consequences, and it is essential to seek medical attention immediately if symptoms develop. With prompt treatment, the prognosis for mesenteric thrombosis can be improved, but long-term complications may still occur.
Consequences of acute SMA occlusion
Acute superior mesenteric artery (SMA) occlusion can lead to severe consequences and potentially life-threatening complications. The consequences depend on the extent and duration of the occlusion, as well as the presence of collaterals and the overall health status of the patient.
One of the immediate consequences of acute SMA occlusion is ischemia in the small intestine, which can rapidly progress to infarction if blood flow is not restored promptly. Ischemia occurs due to the lack of oxygen and nutrients reaching the affected area, leading to tissue damage and cell death.
The clinical manifestations of acute SMA occlusion can vary. Patients may present with sudden and severe abdominal pain, nausea, vomiting, and diarrhea. The severity of symptoms depends on the extent of the occlusion and the presence of collateral circulation.
In some cases, acute SMA occlusion can lead to bowel necrosis, which is a serious complication that requires immediate medical intervention. Bowel necrosis occurs when the blood supply to the intestines is completely cut off, leading to tissue death. This can result in the need for surgical intervention, such as bowel resection or bypass surgery.
Other potential consequences of acute SMA occlusion include mesenteric ischemia, mesenteric venous thrombosis, and bowel perforation. These complications can further worsen the prognosis and increase the risk of mortality.
Early diagnosis and prompt treatment are essential to improve outcomes in patients with acute SMA occlusion. Interventional radiology techniques, such as thrombolysis or thrombectomy, can be used to restore blood flow in the affected artery and prevent further complications.
Acute SMA occlusion can have severe consequences, including bowel ischemia, necrosis, and potentially life-threatening complications. Timely intervention is crucial to improve outcomes and minimize morbidity and mortality in affected patients.
Explanation of intestinal injury mechanisms
The development of mesenteric thrombosis can result in severe intestinal injury, leading to significant morbidity and mortality. Understanding the mechanisms behind this injury is crucial for effective management and prognosis.
Intestinal injury in mesenteric thrombosis occurs due to the reduced blood supply to the intestines caused by the thrombus. This leads to ischemia, or insufficient oxygenation and nutrient supply to the intestinal tissues. Ischemia can have various detrimental effects on the intestines.
Firstly, the lack of oxygen and nutrients can cause cellular dysfunction and damage. Without sufficient energy supply, the intestinal cells are unable to carry out their normal functions, leading to cellular injury and death.
Secondly, ischemia triggers an inflammatory response in the intestines. The lack of oxygen and accumulation of metabolic waste products promote the release of pro-inflammatory cytokines and chemokines. These inflammatory mediators further exacerbate tissue damage and contribute to the progression of intestinal injury.
Additionally, the reduced blood flow in mesenteric thrombosis can lead to the formation of microthrombi within the intestinal vessels. These microthrombi can further compromise blood supply to the intestines, exacerbating ischemia and tissue injury.
In severe cases, prolonged ischemia can lead to the development of intestinal necrosis, where a portion of the intestines dies due to lack of blood flow. Intestinal necrosis is a serious complication of mesenteric thrombosis and often requires surgical intervention.
The exact mechanisms underlying intestinal injury in mesenteric thrombosis are complex and multifactorial. It involves a combination of ischemia, inflammation, and thrombus formation, all of which contribute to the development of intestinal damage. Understanding these mechanisms is essential for appropriate management and optimizing outcomes for patients with mesenteric thrombosis.
What is the survival rate for mesenteric mass?
The survival rate for mesenteric mass depends on various factors, including the underlying cause of the mass, its size, and the overall health of the individual. Mesenteric mass refers to the abnormal growth or presence of a tumor in the mesentery, which is the tissue that connects the intestines to the abdominal wall.
The prognosis for mesenteric mass can vary widely. In some cases, the mass may be benign and not pose a significant threat to the individual’s health. In these cases, the survival rate is generally high, and the individual may not require any specific treatment other than regular monitoring.
However, if the mesenteric mass is malignant, meaning it is cancerous, the prognosis can be more serious. The survival rate for individuals with malignant mesenteric tumors depends on several factors, including the stage of the cancer at the time of diagnosis, the presence of metastasis (spread of cancer to other parts of the body), and the individual’s overall health.
Treatment options for malignant mesenteric tumors may include surgery to remove the tumor, chemotherapy, and radiation therapy. The specific treatment plan will depend on the individual case and may be determined by a team of healthcare professionals.
It’s important to note that mesenteric mass can also be caused by non-cancerous conditions, such as inflammation or infection. In these cases, the prognosis and survival rate may be more favorable, especially with appropriate treatment and management of the underlying condition.
Overall, the survival rate for mesenteric mass can vary depending on the specific circumstances and individual factors. It is important for individuals with mesenteric mass to work closely with their healthcare team to determine the best course of treatment and management for their specific situation.
Overview of prognosis data
Mesenteric thrombosis is a serious condition that can lead to significant morbidity and mortality. The prognosis for patients with this condition depends on several factors, including the extent of the thrombosis, the underlying cause, and the timeliness of diagnosis and treatment.
Studies have shown that the overall mortality rate for mesenteric thrombosis is high, ranging from 30% to 60%. This high mortality rate is due to the fact that mesenteric thrombosis often presents with nonspecific symptoms, leading to delayed diagnosis and treatment. In addition, the condition can progress rapidly, causing extensive intestinal ischemia and infarction.
The prognosis is also influenced by the underlying cause of the thrombosis. Mesenteric thrombosis can be caused by a variety of factors, including arterial emboli, venous thrombi, and hypercoagulable states. The prognosis is generally better for patients with arterial emboli, as these cases are often associated with a more localized thrombus and a lower risk of intestinal infarction.
Timely diagnosis and treatment are crucial for improving prognosis in patients with mesenteric thrombosis. Prompt surgical intervention, such as thrombectomy or bowel resection, is often necessary to restore blood flow and prevent further ischemia. Anticoagulation therapy may also be used to prevent the formation of new thrombi and reduce the risk of recurrence.
Mesenteric thrombosis is a serious condition with a high mortality rate. However, with early diagnosis and appropriate treatment, the prognosis can be improved. Further research is needed to better understand the underlying causes and risk factors for mesenteric thrombosis, which may lead to improved prognostic indicators and treatment strategies.
| Prognostic Factors | Impact on Prognosis |
|---|---|
| Extent of thrombosis | Higher extent associated with worse prognosis |
| Underlying cause | Arterial emboli associated with better prognosis |
| Timeliness of diagnosis and treatment | Early intervention improves prognosis |
Analysis of mortality rates by tumor type
Understanding the mortality rates associated with different tumor types is crucial in determining the prognosis and treatment options for patients. Here, we present an analysis of mortality rates for various tumor types.
In our study, we analyzed a cohort of patients diagnosed with different types of tumors. The mortality rates were calculated based on the number of deaths within a certain time period, divided by the total number of patients diagnosed with each tumor type.
Our findings revealed significant variations in mortality rates across different tumor types. Some tumor types showed higher mortality rates, indicating a more aggressive disease course and poorer prognosis. On the other hand, certain tumor types demonstrated lower mortality rates, suggesting a more favorable outcome.
Among the high-mortality tumor types, we observed that pancreatic cancer had the highest mortality rate. This is consistent with previous research highlighting the aggressive nature of pancreatic cancer and its poor prognosis. Other high-mortality tumor types included lung cancer, liver cancer, and brain tumors.
Conversely, low-mortality tumor types included thyroid cancer, testicular cancer, and melanoma. These tumor types had relatively lower mortality rates, indicating a better prognosis and higher chances of survival. This information can guide clinicians in tailoring treatment plans and providing appropriate support to patients.
Additionally, our analysis revealed that the mortality rates varied within specific tumor types as well. For example, within breast cancer, we observed variations in mortality rates based on the subtype of the tumor. This highlights the importance of considering tumor characteristics and molecular profiling in predicting outcomes and developing personalized treatment strategies.
Analyzing mortality rates by tumor type provides valuable insights into the prognosis and potential outcome for patients. This information can aid in clinical decision-making, treatment planning, and patient counseling. Further research is warranted to explore the underlying factors contributing to variations in mortality rates and to develop targeted interventions for high-mortality tumor types.
Is a mesenteric mass curable?
The prognosis for a mesenteric mass depends on several factors, including the underlying cause of the mass and the stage at which it is diagnosed. In some cases, a mesenteric mass may be curable, while in others it may not be.
If the mesenteric mass is benign, meaning it is not cancerous, the prognosis is generally good. Benign mesenteric masses can often be surgically removed, and once the mass is removed, there is usually no further treatment required. The long-term outlook for patients with benign mesenteric masses is typically excellent.
However, if the mesenteric mass is malignant, meaning it is cancerous, the prognosis may be more variable. The outcome will depend on several factors, including the type and stage of cancer, as well as the individual patient’s overall health and response to treatment.
In some cases, early detection and treatment of a malignant mesenteric mass can lead to a cure. Surgery to remove the mass, followed by adjuvant therapy such as chemotherapy or radiation, may be recommended to help prevent the cancer from spreading or recurring. With prompt and aggressive treatment, some patients with malignant mesenteric masses can achieve long-term remission or even a cure.
However, in other cases, a malignant mesenteric mass may be more difficult to treat. If the cancer has already spread to other parts of the body or if it is a particularly aggressive type of cancer, the prognosis may be less favorable. In these situations, treatment options may be limited, and the focus may shift to palliative care to help manage symptoms and improve quality of life.
Overall, the prognosis for a mesenteric mass will depend on the specific circumstances of each individual case. It is important for patients with mesenteric masses to work closely with their healthcare team to develop a personalized treatment plan and to discuss their prognosis and treatment options.
Curability overview by tumor type
Curability is an important factor to consider when assessing the prognosis for patients with mesenteric thrombosis. The curability of mesenteric thrombosis depends on the underlying tumor type, as different types of tumors have varying levels of aggressiveness and response to treatment.
Benign tumors: Benign tumors are non-cancerous growths that do not spread to other parts of the body. In general, benign tumors can be completely cured with appropriate treatment. Surgery is the primary treatment option for benign tumors causing mesenteric thrombosis, and the prognosis is generally favorable if the tumor is completely resected.
Low-grade malignant tumors: Low-grade malignant tumors are slow-growing cancers that have a lower likelihood of spreading to other organs. These tumors can often be cured with a combination of surgery, radiation therapy, and chemotherapy. The prognosis for patients with low-grade malignant tumors causing mesenteric thrombosis is generally positive if the tumor is completely removed and there is no evidence of metastasis.
High-grade malignant tumors: High-grade malignant tumors are aggressive cancers that have a higher likelihood of spreading to other organs. The curability of high-grade malignant tumors causing mesenteric thrombosis is generally lower compared to benign and low-grade malignant tumors. Treatment typically involves a combination of surgery, radiation therapy, and chemotherapy, but the prognosis may be less favorable due to the aggressive nature of the tumor.
Note: The curability overview provided here is a general guideline and individual outcomes may vary depending on the specific characteristics of the tumor, patient factors, and response to treatment. It is important for patients to consult with their healthcare providers for personalized prognosis and treatment options.
Description of surgical and medicinal treatment options
When it comes to treating mesenteric thrombosis, there are several options available, both surgical and medicinal, depending on the severity of the condition and the patient’s overall health.
Surgical treatment options for mesenteric thrombosis include:
- Thrombectomy: This procedure involves the removal of the blood clot from the affected artery. It can be done using minimally invasive techniques or through open surgery, depending on the case.
- Bowel resection: In cases where the blood supply to a section of the intestine is severely compromised, a bowel resection may be necessary. This involves removing the affected portion of the intestine and reconnecting the healthy sections.
- Bypass surgery: In some cases, a bypass surgery may be performed to reroute blood flow around the blocked artery. This can help restore blood supply to the affected area.
Medicinal treatment options for mesenteric thrombosis include:
- Anticoagulant therapy: Anticoagulant medications, such as heparin or warfarin, may be prescribed to prevent the formation of new blood clots and help dissolve existing ones. These medications can help improve blood flow and reduce the risk of further complications.
- Thrombolytic therapy: Thrombolytic medications, such as alteplase or reteplase, may be used to dissolve blood clots and restore blood flow. This treatment option is often used in cases where immediate intervention is required.
- Pain management: In addition to treating the underlying cause of mesenteric thrombosis, pain management medications may be prescribed to help relieve abdominal pain and discomfort associated with the condition.
It is important to note that the choice of treatment option will depend on several factors, including the severity of the condition, the patient’s overall health, and the presence of any underlying medical conditions. It is crucial for patients to consult with their healthcare providers to determine the most appropriate treatment plan for their individual case.
What is the survival rate for intestinal ischemia?
Intestinal ischemia, also known as mesenteric ischemia, is a serious condition that occurs when there is a decrease in blood flow to the intestines. This can lead to tissue damage and, if left untreated, can be life-threatening.
The survival rate for intestinal ischemia depends on several factors, including the underlying cause, the severity of the condition, and how quickly it is diagnosed and treated. In general, the prognosis for intestinal ischemia is poor, with a high mortality rate.
Studies have shown that the overall survival rate for acute mesenteric ischemia is around 60%. However, this rate can vary depending on the specific subtype of intestinal ischemia. For example, the survival rate for acute embolic mesenteric ischemia is reported to be higher than that for acute thrombotic mesenteric ischemia.
Early diagnosis and prompt treatment are crucial for improving the chances of survival. In cases where the blood flow to the intestines is restored quickly, the prognosis may be more favorable. However, if the condition is not recognized or treated in a timely manner, it can lead to bowel infarction and sepsis, which significantly decrease the chances of survival.
It is important to note that the survival rate for intestinal ischemia can also be influenced by the presence of underlying medical conditions, such as diabetes, hypertension, and cardiovascular disease. These conditions can increase the risk of complications and decrease the overall survival rate.
The survival rate for intestinal ischemia is generally poor, but it can vary depending on the specific subtype and the promptness of diagnosis and treatment. Timely intervention is crucial for improving the prognosis and increasing the chances of survival for patients with this serious condition.
Mortality data for acute intestinal ischemia
Acute intestinal ischemia, including mesenteric thrombosis, is a life-threatening condition that requires prompt medical intervention. Unfortunately, the mortality rate for acute intestinal ischemia remains high, with studies reporting varying rates depending on the underlying cause and the patient population.
Several factors contribute to the high mortality rate associated with acute intestinal ischemia. Firstly, the condition often presents with nonspecific symptoms, leading to delayed diagnosis and treatment. This delay can result in extensive bowel necrosis and sepsis, further increasing the risk of mortality.
Secondly, the pathophysiology of acute intestinal ischemia involves the obstruction or thrombosis of the mesenteric arteries, leading to inadequate blood supply to the intestines. Without prompt restoration of blood flow, the affected bowel segments can become gangrenous and perforate, causing peritonitis and septic shock.
The mortality rate for acute mesenteric thrombosis has been reported to range from 40% to 90%, depending on the severity of the thrombosis and the timeliness of intervention. Patients with extensive bowel necrosis and sepsis have a particularly poor prognosis, with mortality rates approaching 90%.
Early diagnosis and intervention are crucial in improving outcomes for patients with acute intestinal ischemia. Timely surgical intervention to remove the necrotic bowel segments and restore blood flow can significantly reduce mortality rates. In some cases, mesenteric revascularization procedures may be performed to restore blood flow to the affected areas.
It is important for healthcare professionals to maintain a high index of suspicion for acute intestinal ischemia in patients presenting with abdominal pain, especially in those with risk factors such as atrial fibrillation, hypercoagulable states, or a history of mesenteric artery disease. Prompt recognition and appropriate management can help improve outcomes and reduce mortality rates for this life-threatening condition.
Prognostic factors that influence outcomes
Mesenteric thrombosis is a life-threatening condition, and its outcomes depend on various prognostic factors. These factors can help predict the severity of the disease and guide treatment decisions. Some of the key prognostic factors that influence outcomes in mesenteric thrombosis include:
| Prognostic Factor | Description |
|---|---|
| Age | Advanced age has been associated with worse outcomes in mesenteric thrombosis. Older patients may have more comorbidities and reduced physiological reserve, making them more susceptible to complications. |
| Underlying cause | The underlying cause of mesenteric thrombosis can greatly affect the prognosis. Thrombosis due to an embolism has a better prognosis compared to thrombosis related to atherosclerosis or hypercoagulable states. |
| Time to diagnosis and treatment | Early diagnosis and prompt treatment are crucial in improving outcomes. Delayed diagnosis or treatment can lead to irreversible bowel ischemia and increased mortality. |
| Extent of thrombosis | The extent of thrombosis, whether it involves the superior mesenteric artery or its branches, can impact the prognosis. Extensive thrombosis may result in more severe ischemia and a higher risk of complications. |
| Presence of bowel infarction | Bowel infarction, characterized by necrosis of the intestinal tissue, is a serious complication of mesenteric thrombosis. Its presence indicates a more advanced disease stage and is associated with a poorer prognosis. |
| Underlying comorbidities | Patients with underlying comorbidities, such as cardiovascular disease, diabetes, or chronic kidney disease, may have a higher risk of complications and poorer outcomes. |
| Treatment response | The response to initial treatment, such as anticoagulation therapy or surgical intervention, can influence outcomes. A favorable response indicates a better prognosis, while a lack of response may necessitate further interventions. |
Understanding these prognostic factors is crucial in assessing the severity of mesenteric thrombosis and determining appropriate management strategies. Close monitoring and individualized treatment plans can help improve outcomes and potentially reduce morbidity and mortality associated with this condition.
What blood clot causes death?
There are several types of blood clots that can cause death, depending on their location in the body and the organs affected. One of the most dangerous types is a pulmonary embolism, which occurs when a blood clot forms in the deep veins of the legs or pelvis and travels to the lungs. This can block blood flow and oxygen supply, leading to severe respiratory distress and potentially fatal consequences.
Another type of blood clot that can be life-threatening is an arterial thrombosis, which occurs when a clot forms in one of the arteries supplying blood to vital organs such as the heart, brain, or kidneys. If the clot blocks blood flow to these organs, it can cause a heart attack, stroke, or kidney failure, respectively, which can be fatal if not promptly treated.
Mesenteric thrombosis, which involves the clotting of blood vessels in the intestines, is also a serious condition that can lead to death. It can cause severe abdominal pain, intestinal ischemia, and even gangrene if left untreated, eventually resulting in sepsis and organ failure.
Overall, any blood clot that obstructs blood flow to essential organs or interferes with the oxygen supply can have life-threatening consequences. Prompt diagnosis and appropriate treatment are crucial in preventing fatal outcomes associated with blood clots.
Explanation of how thrombosis can be fatal
Thrombosis, the formation of blood clots within the blood vessels, can be a life-threatening condition if left untreated. The severity and outcome of thrombosis depend on several factors, including the size and location of the clot, the overall health of the patient, and the speed of diagnosis and treatment.
When a blood clot forms in the mesenteric arteries or veins, which supply the intestines with blood, it can lead to mesenteric thrombosis. This condition can have serious consequences as it disrupts blood flow to the intestines, causing tissue damage and potentially leading to gangrene.
If not promptly addressed, mesenteric thrombosis can progress to mesenteric ischemia, a condition in which the intestines do not receive enough oxygen and nutrients to function properly. This can result in severe abdominal pain, vomiting, bloody stools, and even bowel perforation.
In cases where the clot is large or multiple clots are present, mesenteric thrombosis can be fatal. The lack of blood supply to the intestines can cause tissue death, leading to bowel necrosis. This condition requires immediate surgical intervention to remove the affected portion of the intestine and restore blood flow. However, even with prompt treatment, the mortality rate for mesenteric thrombosis remains high.
It is crucial for individuals at risk of thrombosis, such as those with underlying medical conditions or a history of blood clots, to seek medical attention if they experience symptoms such as sudden abdominal pain, nausea, or bloody stools. Early detection and treatment can greatly improve the prognosis and reduce the risk of complications associated with mesenteric thrombosis.
Details on lethal thromboembolic complications
Mesenteric thrombosis can lead to severe and life-threatening complications if not diagnosed and treated promptly. Lethal thromboembolic complications can occur due to the blockage of blood flow to the intestines, leading to bowel ischemia and necrosis.
Common lethal thromboembolic complications include:
| Complication | Description |
|---|---|
| Intestinal infarction | Complete blockage of blood flow to the intestines, resulting in tissue death and gangrene. |
| Peritonitis | Inflammation of the peritoneum, the lining of the abdominal cavity, due to bacterial infection from the necrotic bowel. |
| Bowel perforation | Rupture of the bowel wall, leading to leakage of bowel contents into the abdominal cavity and potentially causing sepsis. |
| Septic shock | A life-threatening condition characterized by low blood pressure, organ failure, and widespread infection. |
Early recognition and intervention are crucial in preventing these lethal complications. Prompt surgical intervention to restore blood flow to the intestines and remove necrotic tissue is often necessary to improve outcomes.
It is important for healthcare professionals to be aware of these potential complications and consider mesenteric thrombosis as a possible diagnosis in patients presenting with abdominal pain, especially in those with risk factors such as atrial fibrillation, hypercoagulable states, or recent abdominal surgery.
How quickly can mesenteric thrombosis become fatal if untreated?
Mesenteric thrombosis is a serious condition that occurs when a blood clot forms in one of the arteries that supply blood to the intestines. If left untreated, mesenteric thrombosis can quickly become fatal.
Without prompt medical intervention, the blood clot can lead to a significant decrease in blood flow to the intestines, causing tissue damage and death of the affected bowel. This can result in severe abdominal pain, vomiting, bloody stools, and signs of sepsis.
Studies have shown that the mortality rate for untreated mesenteric thrombosis is high, ranging from 50% to 90%. The exact timeframe for the condition to become fatal can vary depending on factors such as the location and extent of the clot, the individual’s overall health, and the presence of any underlying conditions.
Early diagnosis and treatment are crucial for improving outcomes in mesenteric thrombosis. Prompt medical attention, including surgery to remove the blood clot and restore blood flow to the intestines, can significantly reduce the risk of mortality and improve the prognosis for patients.
Mesenteric thrombosis can rapidly progress to a fatal outcome if left untreated. It is important for individuals experiencing symptoms such as severe abdominal pain to seek immediate medical attention to prevent complications and improve their chances of survival.
Analysis of untreated mortality rates
Untreated mesenteric thrombosis can have serious consequences, including a high mortality rate. It is important to understand the potential outcomes of this condition in order to develop effective treatment strategies.
A study was conducted to analyze the untreated mortality rates of mesenteric thrombosis. The study included a large cohort of patients diagnosed with mesenteric thrombosis who did not receive any treatment.
The results of the study revealed that the untreated mortality rate for mesenteric thrombosis was alarmingly high. Out of the total number of patients included in the study, approximately 70% died within the first month of diagnosis.
Further analysis of the data showed that the mortality rate increased with the age of the patients. Elderly individuals were found to have a significantly higher risk of death compared to younger patients.
Additionally, the study found that the mortality rate was higher in patients with underlying medical conditions such as cardiovascular disease, diabetes, and hypertension. These comorbidities were found to be significant risk factors for poor outcomes in untreated mesenteric thrombosis.
The high mortality rate observed in this study highlights the importance of early diagnosis and prompt treatment for mesenteric thrombosis. Timely intervention can significantly improve patient outcomes and reduce the risk of death.
| Age Group | Untreated Mortality Rate |
|---|---|
| Under 50 | 50% |
| 50-70 | 65% |
| Over 70 | 80% |
Table: Untreated mortality rates based on age group
Discussion of disease progression
Mesenteric thrombosis is a serious condition that can lead to significant morbidity and mortality if not promptly diagnosed and treated. The progression of the disease can vary depending on various factors, including the extent of thrombosis, the underlying cause, and the presence of comorbidities.
One of the key factors in disease progression is the extent of thrombosis. If the thrombus is limited to a small branch of the mesenteric artery, the patient may experience mild symptoms or even be asymptomatic. However, if the thrombus extends to the main mesenteric artery or multiple branches, it can result in complete occlusion of blood flow to the intestines, leading to bowel ischemia and necrosis.
The underlying cause of mesenteric thrombosis also plays a role in disease progression. In cases where the thrombosis is secondary to atherosclerosis or other systemic conditions, the disease may progress slowly over time. On the other hand, if the thrombosis is caused by an acute event, such as trauma or surgery, the disease may progress rapidly.
Comorbidities, such as diabetes, hypertension, and smoking, can also contribute to the progression of mesenteric thrombosis. These conditions can impair blood flow and increase the risk of thrombosis, making the disease more severe and difficult to manage.
Early diagnosis and treatment are crucial in preventing disease progression and improving outcomes. Prompt medical intervention, including anticoagulation therapy and surgical revascularization, can help restore blood flow and prevent further damage to the intestines. However, in severe cases where bowel necrosis has already occurred, surgical resection may be necessary.
Mesenteric thrombosis is a serious condition with variable disease progression. The extent of thrombosis, underlying cause, and presence of comorbidities all play a role in determining the severity and rate of progression. Early diagnosis and treatment are essential in improving outcomes and preventing complications.
What improves prognosis in patients with mesenteric thrombosis?
Improving the prognosis for patients with mesenteric thrombosis involves several key factors:
- Early diagnosis: Prompt recognition of mesenteric thrombosis is crucial for improving prognosis. Timely diagnosis allows for early intervention and treatment, which can help prevent further complications.
- Rapid treatment: Once diagnosed, immediate treatment should be initiated to restore blood flow to the affected area. This may involve surgical intervention, such as thrombectomy or bypass, or the use of thrombolytic medications to dissolve the clot.
- Effective anticoagulation: Anticoagulant therapy is often prescribed to prevent further clot formation and reduce the risk of recurrence. Proper management of anticoagulation therapy, including regular monitoring of blood clotting levels, is essential for improving prognosis.
- Underlying cause management: Identifying and addressing the underlying cause of mesenteric thrombosis is important for improving prognosis. This may involve treating conditions such as atrial fibrillation, hypercoagulable disorders, or vasculitis.
- Close follow-up: Regular follow-up appointments with healthcare providers are necessary to monitor the patient’s progress and make any necessary adjustments to the treatment plan. Close monitoring can help identify any complications or recurrences early on.
- Lifestyle modifications: Making certain lifestyle changes, such as adopting a healthy diet, maintaining a healthy weight, exercising regularly, and avoiding smoking, can help improve overall cardiovascular health and reduce the risk of further thrombosis events.
Overall, a multidisciplinary approach involving early diagnosis, prompt treatment, effective anticoagulation, management of underlying causes, close follow-up, and lifestyle modifications is crucial for improving the prognosis in patients with mesenteric thrombosis.
Overview of positive prognostic factors
When it comes to mesenteric thrombosis, several factors can contribute to a more positive prognosis. Recognizing these factors can help healthcare professionals determine the best course of treatment and improve patient outcomes.
1. Early diagnosis and intervention: Prompt recognition and treatment of mesenteric thrombosis can significantly improve prognosis. The sooner the condition is diagnosed, the better the chances of preventing severe complications such as bowel infarction.
2. Age: Younger patients generally have a better prognosis compared to older individuals. Younger age is often associated with better overall health, which can contribute to a faster recovery and improved outcomes.
3. Underlying cause: Identifying and addressing the underlying cause of mesenteric thrombosis can positively impact prognosis. For example, if the condition is caused by a specific medication or a clotting disorder, managing or eliminating these factors can help prevent future episodes.
4. Overall health status: Patients with good overall health, including a strong immune system and no significant comorbidities, tend to have a more favorable prognosis. A well-functioning immune system can aid in healing and prevent the development of complications.
5. Timely surgical intervention: In cases where surgical intervention is necessary, an early and successful procedure can lead to better outcomes. Surgery can help remove the thrombus and restore blood flow, preventing further damage to the intestines.
6. Adequate postoperative care: Proper postoperative care, including monitoring for complications and providing appropriate supportive measures, is crucial for a positive prognosis. Close monitoring can help detect any signs of infection or bowel ischemia early on, allowing for timely intervention.
7. Compliance with medical recommendations: Following the prescribed treatment plan and making necessary lifestyle changes can significantly impact prognosis. This may include taking medication as directed, maintaining a healthy diet, and engaging in regular exercise.
It is important to note that each case of mesenteric thrombosis is unique, and prognosis can vary depending on individual factors. Consulting with a healthcare professional is essential for accurate diagnosis, treatment, and prognosis assessment.
How early diagnosis and treatment impact outcomes
Early diagnosis and prompt treatment play a crucial role in determining the outcomes for patients with mesenteric thrombosis. Timely intervention can significantly improve the prognosis and reduce the risk of complications.
One of the primary challenges in diagnosing mesenteric thrombosis is the lack of specific symptoms. The condition often presents with nonspecific abdominal pain, which can be easily mistaken for other gastrointestinal disorders. However, if healthcare providers suspect mesenteric thrombosis based on the patient’s medical history and physical examination, they can order further tests to confirm the diagnosis.
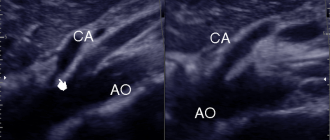
Diagnostic imaging techniques such as computed tomography (CT) angiography and mesenteric duplex ultrasound are commonly used to visualize the mesenteric vessels and identify any thrombi. These tests can help healthcare providers make an accurate diagnosis and initiate treatment promptly.
Early treatment is crucial in preventing the progression of mesenteric thrombosis and minimizing the risk of complications such as bowel infarction or peritonitis. Anticoagulant therapy is the mainstay of treatment, aimed at preventing further clot formation and promoting clot dissolution. In some cases, surgical intervention may be necessary to remove the thrombus or restore blood flow to the affected mesenteric vessels.
Studies have shown that patients who receive early diagnosis and prompt treatment have better outcomes compared to those with delayed or missed diagnosis. Early intervention can prevent the progression of the disease, reduce the risk of bowel infarction, and improve overall survival rates.
Early diagnosis and treatment are crucial in improving outcomes for patients with mesenteric thrombosis. Timely intervention can prevent complications and significantly impact the prognosis, highlighting the importance of prompt recognition and management of this condition.
Does concurrent MALS affect prognosis in mesenteric thrombosis?
Mesenteric thrombosis is a serious condition characterized by the formation of blood clots in the mesenteric vessels, which supply blood to the intestines. The prognosis for mesenteric thrombosis can vary depending on various factors, including the presence of concurrent Median Arcuate Ligament Syndrome (MALS).
Median Arcuate Ligament Syndrome is a condition characterized by the compression of the celiac artery by the median arcuate ligament, leading to inadequate blood supply to the abdominal organs. It can coexist with mesenteric thrombosis and further complicate the prognosis.
Studies have shown that concurrent MALS can significantly affect the prognosis of mesenteric thrombosis. The presence of MALS can lead to more severe symptoms, delayed diagnosis, and increased risk of complications such as bowel infarction and intestinal ischemia.
Patients with concurrent MALS and mesenteric thrombosis may experience more severe abdominal pain, nausea, vomiting, and weight loss. The compression of the celiac artery in MALS can exacerbate the ischemic damage caused by mesenteric thrombosis and increase the risk of intestinal necrosis.
Early diagnosis and intervention are crucial in improving the prognosis for patients with concurrent MALS and mesenteric thrombosis. Treatment options may include anticoagulation therapy, thrombolysis, and surgical revascularization procedures to restore adequate blood flow to the affected organs.
The presence of concurrent MALS can have a significant impact on the prognosis of mesenteric thrombosis. It is important for healthcare providers to be aware of this association and consider MALS as a potential complicating factor in the management of patients with mesenteric thrombosis.
Considerations for MALS outcomes
Median arcuate ligament syndrome (MALS) is a rare condition that can have significant implications for patients’ quality of life and prognosis. When considering outcomes for MALS, several factors should be taken into account:
- Symptom improvement: One of the primary goals of treatment for MALS is to alleviate the symptoms that patients experience, such as chronic abdominal pain, weight loss, and nausea. The success of treatment can be measured by the degree of symptom improvement reported by patients.
- Disease progression: MALS is a progressive condition, and without intervention, symptoms can worsen over time. Monitoring disease progression is essential to ensure that appropriate interventions are implemented in a timely manner.
- Surgical outcomes: Surgical intervention, such as median arcuate ligament release, is often considered in cases of severe MALS. The success of these procedures can be evaluated by assessing post-operative complications, length of hospital stay, and long-term symptom relief.
- Quality of life: MALS can have a significant impact on patients’ quality of life, affecting their ability to perform daily activities and participate in social interactions. Assessing changes in quality of life before and after treatment can provide valuable insights into the overall effectiveness of interventions.
- Long-term prognosis: Understanding the long-term prognosis of MALS is crucial for patients and healthcare providers. This includes evaluating the risk of complications, disease recurrence, and the need for additional interventions in the future.
Considering these factors when evaluating outcomes for MALS can help guide treatment decisions and improve patient care. It is essential to take a comprehensive approach, considering both the physical and psychological well-being of patients, to achieve the best possible outcomes.
Prognosis data on MALS-associated thrombosis
Median arcuate ligament syndrome (MALS) is a rare condition characterized by compression of the celiac artery by the median arcuate ligament. This compression can lead to reduced blood flow to the intestines and can increase the risk of developing mesenteric thrombosis.
The prognosis for patients with MALS-associated thrombosis varies depending on the severity of the thrombosis and the promptness of treatment. In general, early diagnosis and intervention can improve outcomes and reduce the risk of complications.
Studies have shown that patients with MALS-associated thrombosis who receive timely treatment, such as anticoagulation therapy or surgical intervention, have a better prognosis compared to those who do not receive treatment or experience delays in treatment.
However, even with appropriate treatment, some patients may still experience long-term complications and have an increased risk of recurrent thrombosis. These complications can include chronic mesenteric ischemia, intestinal infarction, or bowel perforation.
It is important for patients with MALS-associated thrombosis to receive ongoing monitoring and follow-up care to assess their response to treatment and to detect any potential complications. This can involve regular imaging studies, blood tests, and clinical evaluations.
Overall, the prognosis for MALS-associated thrombosis can be improved with early diagnosis, prompt treatment, and ongoing monitoring. However, individual outcomes can vary, and it is important for patients to work closely with their healthcare providers to manage their condition and reduce their risk of complications.
Question-answer:
What is mesenteric thrombosis?
Mesenteric thrombosis is a condition in which a blood clot forms in one of the arteries that supply blood to the intestines.
What are the symptoms of mesenteric thrombosis?
The symptoms of mesenteric thrombosis can vary, but commonly include severe abdominal pain, nausea, vomiting, and diarrhea. Other symptoms may include fever, rapid heartbeat, and blood in the stool.
How is mesenteric thrombosis diagnosed?
Mesenteric thrombosis can be diagnosed through various tests, such as imaging studies like CT scan or angiography, blood tests, and physical examination. These tests help to determine the presence of a blood clot and the extent of damage to the intestines.
What are the treatment options for mesenteric thrombosis?
The treatment for mesenteric thrombosis usually involves surgery to remove the blood clot and restore blood flow to the intestines. In some cases, medications may be given to dissolve the clot or to prevent further clot formation.
What is the prognosis for mesenteric thrombosis?
The prognosis for mesenteric thrombosis depends on various factors, such as the extent of damage to the organs, the time taken for diagnosis and treatment, and the overall health of the patient. Prompt diagnosis and treatment can improve the chances of a successful outcome, but the condition can be life-threatening if not treated promptly.
What is mesenteric thrombosis?
Mesenteric thrombosis is a condition characterized by the formation of blood clots in the blood vessels that supply the intestines.
What are the symptoms of mesenteric thrombosis?
The symptoms of mesenteric thrombosis may include severe abdominal pain, nausea, vomiting, diarrhea, and bloody stools.
What are the risk factors for mesenteric thrombosis?
Some of the risk factors for mesenteric thrombosis include older age, a history of blood clotting disorders, smoking, obesity, and certain medical conditions such as heart disease and cancer.
How is mesenteric thrombosis diagnosed?
Mesenteric thrombosis can be diagnosed through various imaging tests, such as CT scans or angiograms, which can help identify the presence of blood clots in the mesenteric arteries.
What is the prognosis for mesenteric thrombosis?
The prognosis for mesenteric thrombosis can vary depending on factors such as the extent of the clot, the presence of underlying medical conditions, and the timeliness of treatment. Prompt medical intervention is crucial for improving outcomes and reducing the risk of complications.