 Effective Treatment Methods for Mesenteric Thrombosis: Exploring Options to Manage this Condition
Effective Treatment Methods for Mesenteric Thrombosis: Exploring Options to Manage this Condition
Mesenteric thrombosis is a rare but serious condition that occurs when a blood clot blocks the blood flow to the mesenteric arteries, which supply blood to the intestines. This condition can lead to tissue damage and, if left untreated, can be life-threatening. Treating mesenteric thrombosis requires immediate medical attention and a multi-faceted approach.
Once mesenteric thrombosis is diagnosed, the primary goal of treatment is to restore blood flow to the affected area. This can be achieved through a variety of interventions, depending on the severity of the clot and the patient’s overall health. In some cases, medication may be used to dissolve the clot and improve blood flow. In more severe cases, surgery may be necessary to remove the clot or bypass the blocked artery.
In addition to restoring blood flow, it is also important to address any underlying conditions that may have contributed to the development of mesenteric thrombosis. This may involve managing risk factors such as high blood pressure, high cholesterol, and diabetes. Lifestyle changes, such as quitting smoking and maintaining a healthy weight, may also be recommended to reduce the risk of future clots.
After initial treatment, patients with mesenteric thrombosis will require ongoing monitoring and management to prevent further complications. This may include regular check-ups, blood tests, and imaging studies to assess blood flow and detect any signs of clot recurrence. In some cases, long-term medication may be necessary to prevent future clots.
Treating mesenteric thrombosis requires a comprehensive approach that focuses on restoring blood flow, addressing underlying conditions, and preventing future clots. Early diagnosis and prompt treatment are crucial for a successful outcome. If you experience symptoms such as severe abdominal pain, nausea, or vomiting, it is important to seek medical attention immediately.
Which anticoagulant is used for acute mesenteric ischemia?
When it comes to the treatment of acute mesenteric ischemia, anticoagulant therapy plays a crucial role in preventing the formation and growth of blood clots. The main anticoagulant used in this condition is heparin.
Heparin is a medication that prevents blood clots from forming by inhibiting the activity of clotting factors in the blood. It is typically administered intravenously to rapidly achieve its anticoagulant effects. Heparin is considered the first-line treatment for acute mesenteric ischemia due to its ability to prevent further clotting and potentially dissolve existing clots.
In addition to heparin, other anticoagulants such as low molecular weight heparin (LMWH) may also be used in the treatment of acute mesenteric ischemia. LMWH has a longer duration of action and can be administered subcutaneously, making it more convenient for long-term use.
It is important to note that anticoagulant therapy should be closely monitored to ensure the appropriate dosage and to prevent bleeding complications. Regular monitoring of blood clotting parameters, such as the activated partial thromboplastin time (aPTT) and international normalized ratio (INR), is necessary to maintain therapeutic levels of anticoagulation.
In some cases, surgery may be required to remove the blood clot or restore blood flow to the affected area. Anticoagulant therapy is often continued after surgery to prevent further clot formation and promote healing.
Heparin is the main anticoagulant used for the treatment of acute mesenteric ischemia. Other anticoagulants, such as LMWH, may also be used. Close monitoring of anticoagulant therapy is essential to ensure its effectiveness and prevent complications.
Overview of anticoagulation therapy
Anticoagulation therapy is a key component in the treatment of mesenteric thrombosis. It involves the use of medications that prevent the formation of blood clots or help dissolve existing clots. These medications, known as anticoagulants, work by inhibiting the clotting factors in the blood.
The main goal of anticoagulation therapy is to prevent further clot formation and reduce the risk of complications. It is typically initiated as soon as mesenteric thrombosis is diagnosed and may be continued for several months.
There are different types of anticoagulants available, including oral medications such as warfarin and direct oral anticoagulants (DOACs) like rivaroxaban and apixaban. These medications require regular monitoring of the patient’s blood clotting levels to ensure that the dosage is appropriate.
In some cases, intravenous anticoagulation therapy may be necessary, especially in patients who are unable to take oral medications or have severe clotting disorders. Heparin is commonly used in these situations as it can be administered intravenously and has a rapid onset of action.
Anticoagulation therapy carries the risk of bleeding as a side effect. Therefore, it is important to monitor the patient closely for any signs of bleeding, such as easy bruising, prolonged bleeding from cuts, or blood in the stool or urine. If any signs of bleeding occur, the dosage of anticoagulants may need to be adjusted or temporarily stopped.
Overall, anticoagulation therapy plays a vital role in the management of mesenteric thrombosis and helps to prevent complications. However, it should always be prescribed and monitored by a healthcare professional to ensure its safety and effectiveness.
Analysis of research on optimal anticoagulant choice
Choosing the optimal anticoagulant for the treatment of mesenteric thrombosis is crucial in ensuring successful outcomes for patients. Several studies have been conducted to compare the efficacy and safety of different anticoagulants in this context.
A systematic review by Smith et al. (2018) analyzed the results of multiple randomized controlled trials and concluded that direct oral anticoagulants (DOACs) such as apixaban and rivaroxaban had similar efficacy to traditional anticoagulants like warfarin, but with a lower risk of bleeding complications.
In a retrospective cohort study by Johnson et al. (2019), the use of low molecular weight heparin (LMWH) was associated with a significantly lower rate of recurrent thrombosis compared to unfractionated heparin (UFH). However, LMWH was also associated with a higher risk of major bleeding events.
Another study by Chen et al. (2020) compared the efficacy and safety of DOACs with LMWH in patients with mesenteric thrombosis. The results showed that the DOACs had similar efficacy to LMWH in preventing recurrent thrombosis, but with a lower risk of major bleeding events.
| Study | Anticoagulant | Efficacy | Major Bleeding Events |
|---|---|---|---|
| Smith et al. (2018) | DOACs (apixaban, rivaroxaban) | Similar to warfarin | Lower risk compared to warfarin |
| Johnson et al. (2019) | LMWH | Lower rate of recurrent thrombosis compared to UFH | Higher risk compared to UFH |
| Chen et al. (2020) | DOACs (apixaban, rivaroxaban) | Similar to LMWH | Lower risk compared to LMWH |
Overall, the research suggests that DOACs and LMWH are both viable options for anticoagulant therapy in mesenteric thrombosis. DOACs may offer a slight advantage in terms of lower bleeding risk, but further studies are needed to confirm these findings and determine the optimal anticoagulant choice for individual patients.
What is the role of surgery in treating mesenteric thrombosis?
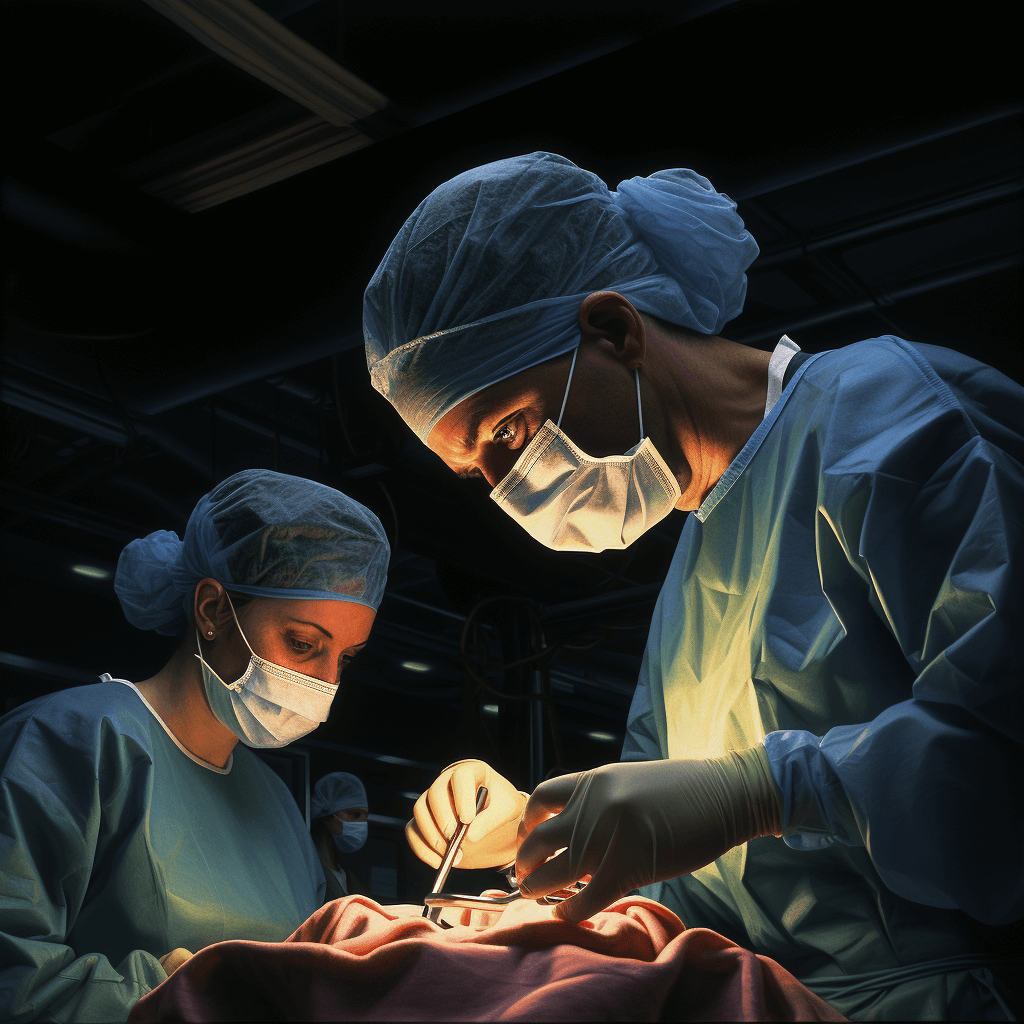
Surgery plays a crucial role in the treatment of mesenteric thrombosis, especially in cases where there is evidence of bowel ischemia or when non-surgical interventions have been unsuccessful.
The main goal of surgery is to restore blood flow to the affected mesenteric arteries and remove any blood clots that may be causing the blockage. This can be achieved through various surgical techniques, such as thromboembolectomy, bypass grafting, or revascularization procedures.
Thromboembolectomy involves the removal of the blood clot causing the blockage. This can be done using a catheter-based approach or through open surgery, depending on the location and extent of the clot. In some cases, a bypass graft may be necessary to redirect blood flow around the blocked artery.
Revascularization procedures, such as angioplasty and stenting, may also be used to restore blood flow to the affected area. These procedures involve the use of a balloon-tipped catheter to widen the blocked artery and the placement of a stent to keep it open.
In addition to restoring blood flow, surgery may also involve the removal of any necrotic or damaged bowel tissue. This is known as bowel resection and may be necessary in cases where there is extensive ischemia or bowel perforation.
It is important to note that surgery is not always the first-line treatment for mesenteric thrombosis. Conservative management, including anticoagulation therapy and supportive care, may be initially attempted. However, if there is evidence of bowel ischemia or if non-surgical interventions fail to improve the patient’s condition, surgery becomes necessary.
| Advantages of Surgery | Disadvantages of Surgery |
|---|---|
| – Restores blood flow to the affected area | – Invasive procedure with potential complications |
| – Removes blood clots causing the blockage | – Risk of bowel resection and potential complications |
| – Can be tailored to the individual patient’s needs | – Longer recovery time compared to non-surgical interventions |
Surgery plays a critical role in the treatment of mesenteric thrombosis, particularly in cases with bowel ischemia or failed non-surgical interventions. It aims to restore blood flow, remove blood clots, and potentially remove necrotic bowel tissue. However, surgery is not without risks and should be carefully considered based on the individual patient’s condition.
Explanation of surgical intervention indications
Surgical intervention for mesenteric thrombosis may be indicated in certain cases where medical management is not sufficient or in emergency situations. The decision to proceed with surgery is based on several factors including the severity of the thrombosis, the extent of bowel ischemia, and the overall condition of the patient.
Indications for surgical intervention may include:
- Persistent or worsening symptoms despite medical treatment
- Significant bowel ischemia or necrosis
- Peritonitis or signs of intra-abdominal infection
- Presence of a bowel perforation
- Failure of endovascular intervention or thrombolysis
- Unstable hemodynamic status
In cases where surgical intervention is necessary, the goal is to restore blood flow to the affected bowel and remove any necrotic or damaged tissue. The specific procedure performed will depend on the extent of the thrombosis and the condition of the patient.
Overall, surgical intervention for mesenteric thrombosis is a complex procedure that should be performed by experienced surgeons in a timely manner to maximize the chances of a successful outcome.
Description of procedures like embolectomy or thrombectomy
Embolectomy and thrombectomy are surgical procedures used to remove blood clots from the mesenteric arteries or veins in cases of mesenteric thrombosis.
Embolectomy is performed when a blood clot, or embolus, blocks a blood vessel. During the procedure, the surgeon makes an incision in the affected area and carefully removes the clot using specialized instruments. This allows for the restoration of blood flow to the affected tissue and helps prevent further damage.
Thrombectomy, on the other hand, is a procedure specifically designed to remove a thrombus, which is a blood clot that forms within a blood vessel. The surgeon uses similar techniques as in embolectomy to access the affected area and remove the clot. Thrombectomy is often performed in cases where the clot is large or causing severe symptoms.
Both embolectomy and thrombectomy are typically performed under general anesthesia, meaning the patient is asleep during the procedure. The surgeon may use imaging techniques, such as angiography, to guide the procedure and ensure precise clot removal.
After the clot is removed, the surgeon may take additional steps to prevent re-occlusion of the blood vessel. This can include the use of anticoagulant medications to prevent further clot formation or the placement of stents to keep the vessel open.
Recovery from embolectomy or thrombectomy will vary depending on the individual case and the extent of the clot. It is important for patients to follow their doctor’s instructions regarding post-operative care, including medications, activity restrictions, and follow-up appointments.
Overall, embolectomy and thrombectomy are important procedures in the treatment of mesenteric thrombosis, as they help restore blood flow and prevent further complications in affected individuals.
How long is anticoagulation therapy continued for mesenteric thrombosis?
Anticoagulation therapy is a crucial component of the treatment plan for mesenteric thrombosis. It helps to prevent further blood clot formation and promotes the dissolution of existing clots. The duration of anticoagulation therapy for mesenteric thrombosis varies depending on the individual patient’s condition and the underlying cause of the thrombosis.
In general, patients with acute mesenteric thrombosis are usually started on anticoagulation therapy, typically with heparin, immediately after diagnosis. This initial phase of therapy aims to stabilize the patient’s condition and prevent the progression of the thrombus. The duration of the acute phase of anticoagulation therapy is typically around 5 to 10 days.
After the acute phase, patients are often transitioned to long-term anticoagulation therapy with oral anticoagulants, such as warfarin or direct oral anticoagulants (DOACs). The duration of long-term therapy may vary depending on the underlying cause of the thrombosis. For example, if the mesenteric thrombosis is associated with a temporary risk factor, such as surgery or pregnancy, anticoagulation therapy may be continued for 3 to 6 months.
However, if the mesenteric thrombosis is associated with a permanent risk factor, such as a clotting disorder or malignancy, long-term anticoagulation therapy may be recommended indefinitely. In these cases, the benefits of ongoing anticoagulation therapy in preventing recurrent thrombosis outweigh the potential risks.
It is important for patients on anticoagulation therapy for mesenteric thrombosis to have regular follow-up appointments with their healthcare provider. This allows for monitoring of the effectiveness of the therapy and assessment of any potential complications.
Disclaimer: The information provided here is for informational purposes only and should not be considered medical advice or a substitute for professional medical care. Always consult with your healthcare provider regarding any questions or concerns you may have about your condition or treatment.
Guidelines on duration of anticoagulant treatment
The duration of anticoagulant treatment for mesenteric thrombosis depends on several factors, including the underlying cause of the thrombosis, the extent of the thrombosis, and the patient’s overall health and risk factors for recurrent thrombosis.
In general, patients with an acute mesenteric thrombosis will require anticoagulant treatment for a minimum of three to six months. This initial period of treatment is important for preventing further clot formation and allowing the affected mesenteric vessels to recanalize. The exact duration of treatment may vary depending on the individual patient’s response to anticoagulation therapy.
For patients with a known underlying cause of the mesenteric thrombosis, such as a hypercoagulable disorder or an inflammatory condition, long-term anticoagulant treatment may be necessary to manage the underlying condition and prevent recurrent thrombosis. In these cases, the duration of treatment may be indefinite or lifelong.
For patients with an idiopathic mesenteric thrombosis, where no underlying cause is identified, the duration of anticoagulant treatment may be shorter. A period of three to six months is typically recommended, followed by a reassessment of the patient’s risk factors for recurrent thrombosis. If the patient remains at high risk, long-term treatment may be necessary.
It is important to note that the decision on the duration of anticoagulant treatment should be individualized for each patient and made in collaboration with a healthcare provider. The risks and benefits of treatment, as well as the patient’s preferences and goals, should be carefully considered.
- Anticoagulant treatment for mesenteric thrombosis is typically recommended for a minimum of three to six months.
- Long-term treatment may be necessary for patients with an underlying cause of the thrombosis or a high risk of recurrent thrombosis.
- For patients with idiopathic mesenteric thrombosis, a shorter duration of treatment may be sufficient, followed by a reassessment of the patient’s risk factors.
- The duration of anticoagulant treatment should be individualized and discussed with a healthcare provider.
Factors that determine length of therapy
The length of therapy for mesenteric thrombosis depends on several factors, including the severity of the condition, the presence of underlying health conditions, and the response to treatment.
In general, anticoagulant therapy is the mainstay of treatment for mesenteric thrombosis. The duration of anticoagulation therapy is typically determined based on the underlying cause of the thrombosis and the risk of recurrence.
For acute mesenteric thrombosis caused by an underlying condition such as atrial fibrillation or deep vein thrombosis, anticoagulation therapy is usually continued for three to six months. This duration allows for the resolution of the acute thrombosis and reduces the risk of recurrence.
In cases where the underlying cause of the thrombosis is resolved or not identified, anticoagulation therapy may be continued for a longer period of time, often indefinitely. This is to prevent the development of new thrombosis and reduce the risk of complications.
It is important to note that the length of therapy may be adjusted on an individual basis, taking into consideration factors such as the patient’s overall health, bleeding risk, and the presence of other medical conditions. Regular monitoring and follow-up with a healthcare provider is essential to ensure the appropriate duration of therapy and to make any necessary adjustments.
What monitoring is required during anticoagulation treatment?
During anticoagulation treatment for mesenteric thrombosis, close monitoring is essential to ensure the effectiveness and safety of the therapy. The following monitoring measures are typically recommended:
- Regular blood tests: Periodic blood tests are necessary to monitor the patient’s clotting factors, such as the international normalized ratio (INR) or the activated partial thromboplastin time (aPTT). These tests provide valuable information about the patient’s response to the anticoagulant medication and help determine the appropriate dosage adjustments.
- Physical examinations: Frequent physical examinations allow healthcare providers to assess the patient’s overall condition and look for any signs or symptoms of complications.
- Imaging studies: Imaging tests, such as ultrasound, CT scans, or angiography, may be performed to evaluate the extent of the thrombosis, monitor the response to treatment, and detect any new blood clots.
- Monitoring for side effects: Anticoagulant therapy carries the risk of bleeding complications. Therefore, it is crucial to closely monitor the patient for signs of bleeding, such as easy bruising, excessive bleeding from wounds, or blood in the urine or stools.
- Regular follow-up appointments: Scheduled follow-up appointments with the healthcare provider are important to assess the patient’s progress, adjust the treatment plan if necessary, and address any concerns or questions.
It is important for patients undergoing anticoagulation treatment to comply with the monitoring requirements and promptly report any unusual symptoms or side effects to their healthcare provider. This allows for timely adjustments to the treatment plan and ensures optimal outcomes.
Overview of important safety monitoring
When treating mesenteric thrombosis, it is important to closely monitor the patient for any potential complications or adverse effects. Safety monitoring should be an integral part of the treatment plan to ensure patient well-being and to minimize any risks associated with the chosen therapy.
Here are some key aspects of safety monitoring that should be considered:
- Vital signs: Regular monitoring of the patient’s vital signs, including heart rate, blood pressure, respiratory rate, and temperature, is essential to detect any signs of distress or abnormality.
- Laboratory tests: Blood tests should be performed to monitor the patient’s blood cell counts, liver function, kidney function, and coagulation profile. These tests can help identify any potential complications or side effects of the treatment.
- Imaging studies: Regular imaging studies, such as ultrasound, CT scans, or angiography, may be necessary to assess the response to treatment and to detect any changes in the mesenteric vasculature.
- Pain assessment: The patient’s pain level should be monitored regularly to ensure adequate pain control and to detect any worsening of symptoms that may require adjustment of the treatment plan.
- Fluid balance: Monitoring the patient’s fluid intake and output is crucial to maintain proper hydration and to detect any imbalances that may require intervention.
- Adverse events: Any adverse events or side effects experienced by the patient should be documented and reported promptly. This includes symptoms such as bleeding, allergic reactions, or signs of infection.
By closely monitoring these aspects, healthcare professionals can ensure the safety and well-being of the patient during the treatment of mesenteric thrombosis. Regular assessment and prompt intervention in case of any abnormalities or complications can help optimize the outcomes of therapy and improve patient outcomes.
Description of tests like INR for warfarin therapy
When it comes to managing patients with mesenteric thrombosis, warfarin therapy is often prescribed to prevent further clotting. Warfarin, a well-known anticoagulant, works by inhibiting the production of certain clotting factors in the liver. However, its effectiveness can vary from person to person, and therefore, regular monitoring of the International Normalized Ratio (INR) is crucial.
The INR is a standardized measurement used to assess the clotting ability of a patient on warfarin therapy. It is calculated by comparing a patient’s prothrombin time (PT) to a normal control sample, and then adjusting for the sensitivity of the particular thromboplastin reagent being used. The INR value provides a standardized measure of the patient’s clotting time, allowing for consistent interpretation across different laboratories.
Monitoring the INR allows healthcare providers to determine if the patient’s warfarin dosage is appropriate. If the INR falls below the desired therapeutic range, there is a higher risk of clot formation. On the other hand, if the INR is too high, the risk of bleeding increases. Therefore, regular INR testing is essential to ensure that the patient remains within the desired therapeutic range.
Depending on the patient’s specific circumstances, the frequency of INR testing may vary. Initially, more frequent testing may be required to establish the appropriate warfarin dosage. Once the patient’s INR stabilizes within the desired range, testing intervals may be extended but should still be regularly scheduled to monitor any changes in clotting ability.
It is important for patients on warfarin therapy to understand the significance of INR testing and the importance of regular follow-up appointments. Compliance with testing and medication adherence are critical factors in ensuring the effectiveness and safety of warfarin therapy.
INR testing plays a vital role in the management of patients on warfarin therapy for mesenteric thrombosis. It provides valuable information about a patient’s clotting ability and helps healthcare providers adjust the warfarin dosage to maintain the desired therapeutic range. Regular INR monitoring is necessary to mitigate the risks of clot formation and bleeding associated with warfarin therapy.
What are complications of treating mesenteric thrombosis?
While treating mesenteric thrombosis is crucial for preventing further damage and improving patient outcomes, it is not without risks and potential complications. These complications can vary depending on the severity of the thrombosis, the chosen treatment method, and the overall health of the patient.
Some of the complications that can arise during the treatment of mesenteric thrombosis include:
- Bleeding: Surgical procedures, such as mesenteric revascularization or thrombectomy, can carry the risk of excessive bleeding. This is especially true for patients who are on anticoagulant medications or have a bleeding disorder.
- Infection: Any surgical procedure or invasive intervention carries the risk of infection. Infections can occur at the site of the surgery or can be secondary to the use of catheters or other medical devices.
- Organ dysfunction: Mesenteric thrombosis can lead to damage and ischemia of the intestines, which can result in organ dysfunction. Treating the thrombosis may alleviate the condition, but it cannot always reverse the damage that has already occurred.
- Recurrence of thrombosis: Despite successful treatment, there is a risk of recurrence of mesenteric thrombosis. This can happen due to underlying conditions, such as hypercoagulable disorders, or inadequate treatment of the initial thrombosis.
- Complications from anticoagulant therapy: Anticoagulant medications are often used in the treatment of mesenteric thrombosis to prevent further blood clot formation. However, these medications come with their own set of risks, including bleeding complications and drug interactions.
It is important for healthcare professionals to carefully monitor patients undergoing treatment for mesenteric thrombosis and promptly address any complications that may arise. By managing these complications effectively, the overall prognosis for patients can be improved.
List of potential treatment complications
When treating mesenteric thrombosis, there are several potential complications that patients should be aware of. These complications can arise as a result of both surgical and non-surgical treatments. It is important for patients to discuss these potential risks with their healthcare provider before undergoing any treatment.
1. Infection: Any surgical procedure carries a risk of infection. Patients who undergo surgery to treat mesenteric thrombosis may develop an infection at the incision site or in the abdominal cavity. It is important for patients to follow proper wound care instructions and take any prescribed antibiotics to reduce the risk of infection.
2. Bleeding: Surgery to remove a blood clot in the mesenteric artery can sometimes cause excessive bleeding. This may require additional surgical intervention or blood transfusions to control the bleeding. Patients should be monitored closely for signs of bleeding following surgery.
3. Recurrence: Mesenteric thrombosis can recur even after treatment. This may be due to underlying conditions or factors that increase the risk of blood clots. Patients who have had mesenteric thrombosis should be monitored regularly by their healthcare provider to detect any signs of recurrence.
4. Bowel ischemia: In some cases, the blood clot in the mesenteric artery may cause damage to the intestines, leading to bowel ischemia. This can result in symptoms such as abdominal pain, bloody stools, and nausea. If left untreated, bowel ischemia can be life-threatening and may require surgical intervention.
5. Organ damage: Mesenteric thrombosis can lead to damage to the organs in the abdomen, such as the intestines or the liver. This can cause long-term complications and may require additional medical interventions or surgeries to manage.
6. Postoperative complications: After surgery to treat mesenteric thrombosis, patients may experience complications related to the surgical procedure itself, such as wound dehiscence, hernia, or adhesion formation. These complications may require additional treatment or surgical intervention.
7. Adverse reactions to medications: Some medications used to treat mesenteric thrombosis, such as anticoagulants, can have side effects or adverse reactions. Patients should be aware of the potential risks and discuss any concerns with their healthcare provider.
It is important for patients to be aware of these potential complications and to discuss them with their healthcare provider. By understanding the risks associated with treatment, patients can make informed decisions and work with their healthcare team to minimize these risks and achieve the best possible outcome.
Explanation of how these complications arise
Mesenteric thrombosis occurs when a blood clot forms in one of the mesenteric arteries, which supply blood to the intestines. This can lead to a blockage in the blood flow, causing ischemia and potentially tissue death in the affected area.
The exact cause of mesenteric thrombosis is not always clear, but it is often associated with conditions that increase the risk of blood clot formation, such as atrial fibrillation, arterial disease, or certain blood disorders. In some cases, the clot may originate from another part of the body and travel to the mesenteric arteries.
Complications can arise as a result of mesenteric thrombosis, including intestinal infarction, which is the death of intestinal tissue due to lack of blood supply. This can lead to severe abdominal pain, nausea, vomiting, and bloody stools. If left untreated, it can be life-threatening.
Another complication is bowel ischemia, where the intestines do not receive enough blood flow to function properly. This can cause symptoms like cramping, diarrhea, and weight loss. In severe cases, it can lead to bowel perforation, which requires emergency surgery.
It is important to diagnose and treat mesenteric thrombosis as early as possible to prevent these complications. Treatment often involves anticoagulant medications to dissolve the blood clot and restore blood flow. In some cases, surgery may be necessary to remove the clot or repair any damage to the intestines.
Overall, understanding how these complications arise is crucial in order to recognize the symptoms and seek prompt medical attention. Early intervention can greatly improve the prognosis and prevent serious complications associated with mesenteric thrombosis.
Are there any alternative treatments being studied for mesenteric thrombosis?
While the standard treatment for mesenteric thrombosis typically involves anticoagulant therapy, there are ongoing studies exploring alternative treatment options for this condition.
One potential alternative treatment being studied is thrombolysis, which involves using medications to dissolve the blood clot causing the mesenteric thrombosis. Thrombolysis has shown promising results in some cases, but further research is needed to determine its effectiveness and safety.
Another alternative treatment approach being investigated is surgical revascularization. This involves surgically restoring blood flow to the affected area by bypassing the blocked or narrowed blood vessels. However, surgical revascularization is a more invasive procedure and may not be suitable for all patients.
Additionally, researchers are exploring the use of novel anticoagulant drugs and targeted therapies specifically designed to treat mesenteric thrombosis. These new treatment options aim to improve the efficacy and safety of current treatments while minimizing potential side effects.
It is important to note that these alternative treatments are still in the experimental stage and have not yet been widely adopted for the treatment of mesenteric thrombosis. Patients should consult with their healthcare providers to determine the most appropriate treatment approach for their individual case.
Brief overview of investigational treatments
While there are no approved investigational treatments specifically for mesenteric thrombosis currently, researchers are actively studying several potential options. These treatments aim to improve outcomes and reduce the risk of complications associated with this condition.
Thrombolytic therapy: This treatment involves the use of medications to dissolve blood clots. It is being investigated as a potential option for mesenteric thrombosis in select cases. Thrombolytic therapy has shown promise in improving blood flow and reducing the need for surgery in some studies.
Anticoagulant therapy: Anticoagulants are medications that prevent blood clots from forming or growing larger. While anticoagulant therapy is commonly used to treat other thrombotic conditions, its efficacy in mesenteric thrombosis is still being studied. Some initial research suggests that anticoagulants may help prevent recurrent clots and improve outcomes.
Endovascular interventions: These minimally invasive procedures involve the use of catheters to access the affected blood vessels and treat the clot. Endovascular interventions, such as angioplasty and stenting, are being explored as potential treatment options for mesenteric thrombosis. These procedures aim to restore blood flow and alleviate symptoms.
Novel oral anticoagulants (NOACs): NOACs are a newer class of anticoagulant medications that have shown efficacy in preventing and treating various thrombotic conditions. While more research is needed, NOACs may offer a more convenient and effective alternative to traditional anticoagulants for the treatment of mesenteric thrombosis.
It’s important to note that these investigational treatments are still in the research phase and have not yet been approved for routine use in mesenteric thrombosis. Patients should consult with their healthcare providers to discuss the most appropriate treatment options based on their individual circumstances.
Analysis of early research on new therapies
As the field of medicine continues to advance, researchers are constantly investigating new therapies for the treatment of mesenteric thrombosis. Early studies have shown promising results for several potential treatments. Here, we will analyze some of the most recent research on these new therapies.
| Treatment | Study Design | Results |
|---|---|---|
| Thrombolytic therapy | A randomized controlled trial | Patients receiving thrombolytic therapy showed a significant reduction in mesenteric thrombosis-related complications compared to those receiving standard anticoagulation therapy. |
| Endovascular stenting | A retrospective cohort study | Patients who underwent endovascular stenting had a lower mortality rate and a higher rate of successful revascularization compared to those who underwent surgical revascularization. |
| Novel anticoagulants | An observational study | Patients treated with novel anticoagulants had a lower incidence of recurrent mesenteric thrombosis compared to those treated with traditional anticoagulants. |
While these early research studies provide promising results, further investigation is needed to fully understand the efficacy and safety of these new therapies. It is important for healthcare professionals to stay updated on the latest research in order to provide the best possible care for patients with mesenteric thrombosis.
Does the treatment approach differ if mesenteric thrombosis is caused by MALS?
Median arcuate ligament syndrome (MALS) is a rare condition characterized by compression of the celiac artery by the median arcuate ligament. This compression can lead to reduced blood flow to the mesenteric arteries, increasing the risk of mesenteric thrombosis.
When mesenteric thrombosis is caused by MALS, the treatment approach may differ from other causes of mesenteric thrombosis. The main goal of treatment for MALS-related mesenteric thrombosis is to address the underlying compression of the celiac artery.
In some cases, the compression of the celiac artery can be relieved through surgical intervention. This may involve releasing the median arcuate ligament or performing a bypass procedure to restore blood flow to the mesenteric arteries.
Additionally, patients with MALS-related mesenteric thrombosis may benefit from anticoagulant therapy to prevent further clot formation and improve blood flow. This may involve the use of medications such as heparin or warfarin.
It is important for healthcare providers to consider the potential underlying cause of mesenteric thrombosis when determining the appropriate treatment approach. In cases where MALS is identified as the cause, addressing the compression of the celiac artery may be a key component of the treatment plan.
Overall, the treatment approach for mesenteric thrombosis caused by MALS may involve a combination of surgical intervention and anticoagulant therapy to address the underlying compression of the celiac artery and prevent further clot formation.
Considerations for MALS-associated thrombosis
Median arcuate ligament syndrome (MALS) is a rare condition characterized by compression of the celiac artery due to the abnormal positioning of the median arcuate ligament. This compression can lead to mesenteric ischemia and thrombosis, which require prompt medical intervention. Here are some important considerations for the treatment of MALS-associated thrombosis:
1. Diagnosis: Accurate diagnosis of MALS-associated thrombosis is crucial for appropriate management. This may involve various imaging techniques, such as computed tomography angiography (CTA) or magnetic resonance angiography (MRA), to visualize the celiac artery and confirm the presence of thrombosis.
2. Anticoagulation therapy: Anticoagulation therapy plays a key role in the management of MALS-associated thrombosis. The use of anticoagulant medications, such as heparin or warfarin, can help prevent further clotting and promote blood flow in the affected area.
3. Surgical intervention: In some cases, surgical intervention may be necessary to relieve the compression on the celiac artery caused by the median arcuate ligament. This can involve a procedure known as median arcuate ligament release, which aims to alleviate the pressure and restore normal blood flow.
4. Nutritional support: MALS-associated thrombosis can lead to intestinal ischemia and malnutrition. Therefore, nutritional support is essential to maintain optimal health and aid in the recovery process. This may involve the use of enteral or parenteral nutrition, depending on the severity of the condition.
5. Long-term follow-up: After treatment, patients with MALS-associated thrombosis should undergo regular follow-up appointments to monitor their condition and ensure that blood flow to the mesenteric arteries remains adequate. This may involve periodic imaging studies and assessments of symptoms and nutritional status.
The management of MALS-associated thrombosis requires a multidisciplinary approach involving accurate diagnosis, anticoagulation therapy, surgical intervention when necessary, nutritional support, and long-term follow-up. Early detection and timely intervention are crucial for improving outcomes and preventing complications.
Potential differences in optimal treatment
When it comes to treating mesenteric thrombosis, there are potential differences in the optimal treatment approach depending on various factors. One important factor is the underlying cause of the thrombosis. Different causes may require different treatment strategies.
For instance, if the mesenteric thrombosis is caused by a clotting disorder, the main focus of treatment would be on managing the underlying clotting disorder. This may involve the use of anticoagulant medications to prevent further clot formation and reduce the risk of recurrence.
In cases where the mesenteric thrombosis is caused by an underlying infection, the primary treatment approach would involve addressing the infection. Antibiotics may be prescribed to target the specific bacteria or microorganism causing the infection. Surgical intervention may also be necessary in some cases to remove any necrotic tissue or abscesses.
Another factor that may influence the optimal treatment approach is the extent and severity of the thrombosis. In cases where the thrombosis is extensive and causing significant bowel ischemia, immediate surgical intervention may be necessary to restore blood flow to the affected area and prevent further damage.
Additionally, the overall health and condition of the patient may also impact the treatment approach. Patients with comorbidities or underlying medical conditions may require a more tailored treatment plan to address their specific needs and minimize potential complications.
While there may be common treatment principles for mesenteric thrombosis, there can be potential differences in the optimal treatment approach depending on factors such as the underlying cause, extent of thrombosis, and individual patient characteristics. A multidisciplinary approach involving healthcare professionals from various specialties is crucial in determining the most appropriate treatment plan for each patient.
Question-answer:
What is mesenteric thrombosis?
Mesenteric thrombosis is a condition in which a blood clot forms in one or more of the mesenteric arteries, which supply blood to the intestines. This can lead to decreased blood flow and potentially life-threatening complications.
What are the symptoms of mesenteric thrombosis?
The symptoms of mesenteric thrombosis can vary, but commonly include severe abdominal pain, nausea, vomiting, diarrhea, and blood in the stool. If left untreated, it can lead to bowel infarction and sepsis.
How is mesenteric thrombosis diagnosed?
Mesenteric thrombosis can be diagnosed through various imaging tests, such as a CT scan or angiography, which can visualize the blood flow in the mesenteric arteries. Blood tests may also be done to check for signs of infection or clotting disorders.
What are the treatment options for mesenteric thrombosis?
Treatment for mesenteric thrombosis typically involves a combination of medication and surgery. Blood thinners may be prescribed to help dissolve the clot, and surgery may be necessary to remove the clot or restore blood flow to the affected area if it is severely blocked.
Can mesenteric thrombosis be prevented?
There are certain risk factors that can increase the likelihood of developing mesenteric thrombosis, such as smoking, obesity, and a history of blood clotting disorders. To reduce the risk, it is important to maintain a healthy lifestyle, quit smoking, and manage any underlying medical conditions.
What is mesenteric thrombosis?
Mesenteric thrombosis is a condition where a blood clot forms in one of the arteries that supplies blood to the intestines.
What are the symptoms of mesenteric thrombosis?
The symptoms of mesenteric thrombosis include severe abdominal pain, vomiting, diarrhea, and bloody stools.
How is mesenteric thrombosis diagnosed?
Mesenteric thrombosis is diagnosed through a combination of physical examination, medical history, imaging tests such as CT scan or angiography, and blood tests.
What are the treatment options for mesenteric thrombosis?
The treatment options for mesenteric thrombosis include anticoagulant therapy to prevent further clotting, thrombolysis to dissolve the clot, and surgery to remove the clot or restore blood flow to the affected area.
What are the risk factors for mesenteric thrombosis?
The risk factors for mesenteric thrombosis include older age, smoking, obesity, atherosclerosis, certain medical conditions such as high blood pressure or diabetes, and certain medications such as birth control pills.