 Advancements in Ultrasound Diagnosis for the Detection and Treatment of Gynecological Disorders
Advancements in Ultrasound Diagnosis for the Detection and Treatment of Gynecological Disorders
Gynecological diseases affect millions of women worldwide and have a significant impact on their reproductive health. Early and accurate diagnosis is crucial for effective treatment and improved outcomes. Ultrasound imaging has emerged as a valuable tool in the diagnosis of gynecological diseases, providing non-invasive and detailed visualizations of the pelvic organs.
Ultrasound, also known as sonography, uses high-frequency sound waves to create images of the internal structures of the body. In gynecology, ultrasound can be used to evaluate the uterus, ovaries, fallopian tubes, and other pelvic organs. It can help detect and diagnose a wide range of conditions, including uterine fibroids, ovarian cysts, endometriosis, and pelvic inflammatory disease.
One of the main advantages of ultrasound is its ability to provide real-time imaging, allowing gynecologists to visualize the pelvic organs in motion. This dynamic imaging capability is particularly useful for assessing the function and movement of the uterus and ovaries, as well as for monitoring the growth and development of a fetus during pregnancy.
In addition to its diagnostic utility, ultrasound is also a safe and cost-effective imaging modality. It does not use ionizing radiation, making it suitable for repeated examinations and monitoring. Furthermore, ultrasound is widely available and relatively affordable, making it accessible to patients in different healthcare settings.
Ultrasound imaging plays a crucial role in the diagnosis of gynecological diseases. Its non-invasive nature, real-time imaging capability, and safety make it an invaluable tool for gynecologists in evaluating and managing various conditions. With ongoing advancements in technology, ultrasound is expected to continue to evolve and improve, further enhancing its diagnostic capabilities in the field of gynecology.
Uterine Conditions
The uterus is a vital organ in the female reproductive system. It is responsible for supporting the growth and development of a fetus during pregnancy. Ultrasound imaging is commonly used to diagnose and monitor various uterine conditions.
Some common uterine conditions that can be detected using ultrasound include:
| Condition | Description | Ultrasound |
| Fibroids | Fibroids are noncancerous growths that develop in or on the uterus. They can vary in size and location and may cause symptoms such as heavy menstrual bleeding, pelvic pain, and infertility. | Ultrasound can detect the presence, size, and location of fibroids. They appear as well-defined masses with variable echogenicity. |
| Polyps | Uterine polyps are small, benign growths that develop in the lining of the uterus. They can cause abnormal uterine bleeding and infertility. | Ultrasound can visualize polyps as soft tissue masses protruding into the uterine cavity. They may appear as hypoechoic or hyperechoic structures. |
| Adenomyosis | Adenomyosis is a condition where the endometrial tissue grows into the muscular wall of the uterus. It can cause heavy menstrual bleeding, pelvic pain, and enlarged uterus. | Ultrasound can show diffuse thickening of the uterine wall, presence of myometrial cysts, and heterogeneity of the myometrium. |
| Endometrial Hyperplasia | Endometrial hyperplasia is an abnormal thickening of the lining of the uterus. It can be a precursor to endometrial cancer. | Ultrasound can reveal focal or diffuse thickening of the endometrium. It can also help in assessing the presence of polyps or masses. |
| Uterine Cancer | Uterine cancer is the abnormal growth of cells in the uterus. It can cause abnormal uterine bleeding, pelvic pain, and enlarged uterus. | Ultrasound can show thickening of the endometrium, presence of masses or polyps, and invasion of adjacent structures. |
Ultrasound is a valuable tool in diagnosing and evaluating various uterine conditions. It can provide detailed information about the size, location, and characteristics of uterine abnormalities, aiding in the development of appropriate treatment plans.
Fibroids
Fibroids, also known as uterine leiomyomas, are noncancerous growths that develop in the uterus. They are made up of muscle and fibrous tissue and can vary in size, ranging from very small to large. Fibroids are a common condition, affecting many women during their reproductive years.
The exact cause of fibroids is unknown, but they are thought to be influenced by hormones, particularly estrogen and progesterone. Factors such as age, family history, and race can also increase the risk of developing fibroids.
Most fibroids do not cause any symptoms and are often discovered during routine pelvic exams or imaging tests. However, some women may experience symptoms such as heavy or prolonged menstrual bleeding, pelvic pain or pressure, frequent urination, and difficulty getting pregnant.
Ultrasound is a commonly used imaging technique to diagnose and monitor fibroids. It uses sound waves to create images of the uterus and can accurately identify the location, size, and number of fibroids. This information is essential for determining the appropriate treatment approach.
Treatment options for fibroids depend on various factors, including the symptoms, the size and location of the fibroids, and the woman’s desire for future pregnancy. Treatment options may include medication to regulate menstrual bleeding, hormonal therapy to shrink the fibroids, or surgical procedures such as myomectomy (removal of the fibroids) or hysterectomy (removal of the uterus).
Fibroids are noncancerous growths that can develop in the uterus. They are a common condition and can cause symptoms such as heavy menstrual bleeding and pelvic pain. Ultrasound is an important tool for diagnosing and monitoring fibroids, and treatment options depend on various factors.
Endometrial polyps
Endometrial polyps are common benign growths that occur in the lining of the uterus, known as the endometrium. They are typically small, finger-like projections that attach to the uterine wall and can vary in size, ranging from a few millimeters to several centimeters in diameter.
Endometrial polyps are often asymptomatic, meaning they do not cause any noticeable symptoms. However, some women may experience abnormal uterine bleeding, such as heavy or prolonged menstrual periods, bleeding between periods, or postmenopausal bleeding. Other possible symptoms include pelvic pain or pressure.
Ultrasound is an effective tool for diagnosing endometrial polyps. Transvaginal ultrasound, which involves inserting a small probe into the vagina, allows for a detailed examination of the uterus and endometrium. The ultrasound images can show the presence of polyps and provide information about their size, location, and number.
Typically, endometrial polyps appear as hypoechoic or isoechoic structures within the endometrial cavity. They may have a smooth or irregular surface and can be sessile (attached directly to the uterine wall) or pedunculated (attached by a stalk). Doppler ultrasound can be used to assess the blood flow within the polyp.
In some cases, endometrial polyps may need to be further evaluated or treated. This can be done through hysteroscopy, a procedure in which a thin, lighted tube is inserted into the uterus to directly visualize the polyps and potentially remove them. Histopathological examination of the polyp tissue can provide a definitive diagnosis and rule out any malignant changes.
Ultrasound plays a crucial role in the diagnosis of endometrial polyps. It allows for the identification and characterization of these benign growths, helping clinicians determine the appropriate management approach for each individual patient.
Adenomyosis
Adenomyosis is a gynecological condition in which the inner lining of the uterus, known as the endometrium, grows into the muscular wall of the uterus. This can cause the uterus to become enlarged and tender, leading to symptoms such as heavy or prolonged menstrual bleeding, severe menstrual cramps, and pelvic pain.
Ultrasound imaging is a valuable tool for diagnosing adenomyosis. It can help to identify the characteristic features of the condition, such as thickening of the uterine wall, the presence of small cysts within the wall, and an irregular border between the endometrium and myometrium.
Transvaginal ultrasound is the preferred imaging technique for evaluating adenomyosis. It involves the insertion of a small ultrasound probe into the vagina, allowing for a detailed examination of the uterus. The probe emits high-frequency sound waves that create images of the pelvic organs, including the uterus.
During the ultrasound examination, the sonographer or radiologist will assess the size and shape of the uterus, as well as the thickness of the uterine wall. They will also look for any abnormalities, such as the presence of cysts or fibroids. The blood flow to the uterus may also be evaluated using a technique called Doppler ultrasound.
In addition to ultrasound, other imaging modalities such as magnetic resonance imaging (MRI) may be used to further evaluate suspected cases of adenomyosis. MRI can provide detailed images of the uterus and help to differentiate adenomyosis from other conditions that may cause similar symptoms.
Overall, ultrasound imaging plays a crucial role in the diagnosis of adenomyosis. It allows for a non-invasive evaluation of the uterus and helps to guide further management decisions. Early detection and accurate diagnosis of adenomyosis can lead to appropriate treatment and improved outcomes for patients.
Uterine cancer
Uterine cancer, also known as endometrial cancer, is a type of cancer that starts in the lining of the uterus. It is the most common type of gynecological cancer and mainly affects postmenopausal women.
There are several risk factors that can increase the likelihood of developing uterine cancer, including obesity, diabetes, high blood pressure, and hormone imbalances. Additionally, women who have never been pregnant or have a history of certain types of ovarian tumors may have an increased risk.
One of the key ways to diagnose uterine cancer is through ultrasound imaging. Transvaginal ultrasound is often used to evaluate the thickness of the endometrium, which can be an indicator of cancer. During the procedure, a probe is inserted into the vagina to obtain detailed images of the uterus and surrounding structures.
If uterine cancer is suspected, further tests such as a biopsy may be performed to confirm the diagnosis. Treatment options for uterine cancer depend on various factors, including the stage of the cancer, the woman’s age, and her overall health. Treatment may involve surgery, radiation therapy, chemotherapy, or a combination of these approaches.
Regular screenings and early detection are important for improving the prognosis of uterine cancer. If you experience any symptoms such as abnormal vaginal bleeding, pelvic pain, or changes in urinary or bowel habits, it is important to seek medical attention promptly.
Overall, ultrasound imaging plays a crucial role in the diagnosis and management of uterine cancer. It allows healthcare professionals to accurately assess the condition of the uterus and guide appropriate treatment decisions.
Ovarian Conditions
Ultrasound imaging is a valuable tool for evaluating various ovarian conditions. It allows for non-invasive visualization of the ovaries and can help diagnose and monitor a range of gynecological diseases.
Ovarian cysts: Ultrasound can detect and characterize ovarian cysts, which are fluid-filled sacs that can develop on or within the ovaries. Ultrasound can help determine the size, location, and composition of the cysts, as well as assess their potential for malignancy.
Ovarian tumors: Ultrasound can aid in the detection and characterization of ovarian tumors, including both benign and malignant tumors. It can provide information about the size, location, and appearance of the tumors, which can help guide further diagnostic and treatment decisions.
Polycystic ovary syndrome (PCOS): Ultrasound is commonly used to diagnose PCOS, a hormonal disorder characterized by enlarged ovaries with multiple small cysts. Ultrasound can help visualize the ovaries and assess their size and appearance, as well as evaluate the presence of other associated features, such as an increased number of follicles.
Ovarian torsion: Ultrasound can assist in the diagnosis of ovarian torsion, a condition in which the ovary twists on its own blood supply, leading to severe pain and potential loss of the ovary. Ultrasound can help identify the twisted ovary and assess blood flow to the affected area, aiding in prompt diagnosis and treatment.
Ovarian cancer: Ultrasound is one of the primary imaging modalities used in the evaluation of ovarian cancer. It can help identify ovarian masses, assess their characteristics, and guide biopsy or surgical interventions. Ultrasound can also be used for monitoring the response to treatment and detecting any potential recurrence of the disease.
Other ovarian conditions: Ultrasound can also be used to evaluate other ovarian conditions, such as ovarian abscesses, endometriomas, and ovarian fibroids. It can provide valuable information about the size, location, and appearance of these conditions, aiding in their diagnosis and management.
Ultrasound imaging plays a crucial role in the diagnosis and management of various ovarian conditions. It allows for non-invasive visualization of the ovaries and provides valuable information about their size, appearance, and characteristics. Ultrasound can aid in the diagnosis of ovarian cysts, tumors, PCOS, ovarian torsion, ovarian cancer, and other ovarian conditions, facilitating appropriate treatment and monitoring of these conditions.
Ovarian cysts
Ovarian cysts are fluid-filled sacs or pockets that develop within or on the surface of the ovaries. They are common and can occur at any age, although they are most commonly found during a woman’s reproductive years.
Ovarian cysts can vary in size, ranging from as small as a pea to as large as a grapefruit. Most ovarian cysts are benign, meaning they are not cancerous, and often go away on their own without treatment. However, some cysts may cause symptoms or complications and require medical intervention.
There are several types of ovarian cysts, including:
- Follicular cysts: These cysts form when the sac on the ovary that should release the egg does not break open to release the egg. This causes the sac to continue growing, forming a cyst.
- Corpus luteum cysts: These cysts form when the sac on the ovary that released the egg reseals and fills with fluid. They usually go away on their own within a few weeks.
- Dermoid cysts: These cysts form from cells that produce human eggs. They can contain tissue, such as hair, skin, or teeth, and are usually benign.
- Endometriomas: These cysts form when tissue similar to the lining of the uterus grows outside the uterus and attaches to the ovary. They are often associated with endometriosis.
Symptoms of ovarian cysts can vary depending on the size and type of the cyst. Some common symptoms include pelvic pain or pressure, bloating, changes in menstruation, and frequent urination.
Ultrasound is commonly used to diagnose ovarian cysts. It allows doctors to visualize the ovaries and determine the size, location, and characteristics of the cyst. In some cases, additional imaging tests or procedures may be necessary to further evaluate the cyst or rule out other conditions.
Treatment for ovarian cysts depends on several factors, including the size and type of the cyst, as well as the presence of symptoms or complications. Small, asymptomatic cysts may simply be monitored over time, while larger cysts or those causing symptoms may require medication or surgery.
Ovarian cysts are common and can vary in size and type. While most cysts are benign and resolve on their own, some may require medical intervention. Ultrasound is an important tool in diagnosing and evaluating ovarian cysts.
Polycystic ovary syndrome
Polycystic ovary syndrome (PCOS) is a common hormonal disorder among women of reproductive age. It is characterized by the presence of multiple cysts in the ovaries, irregular menstrual cycles, and high levels of androgens, or male hormones, in the body.
Ultrasound imaging is an important tool for diagnosing PCOS. The ultrasound scan can reveal the presence of multiple small cysts in the ovaries, usually arranged around the periphery. These cysts are typically small and do not cause any symptoms. In addition to cysts, the ultrasound may also show an increased ovarian volume and a thickened ovarian capsule.
Other features that may be observed on ultrasound include an increased number of follicles, or fluid-filled sacs, within the ovaries, and a characteristic “string of pearls” appearance. The string of pearls refers to a chain of small cysts lined up in a row, which is a classic finding in PCOS.
In addition to aiding in the diagnosis of PCOS, ultrasound can also help in monitoring the response to treatment. For example, if a woman with PCOS is undergoing fertility treatment, ultrasound can be used to assess the growth and development of follicles in the ovaries.
Ultrasound imaging plays a crucial role in the diagnosis and management of polycystic ovary syndrome. It allows for the visualization of cysts, follicles, and other characteristic features of PCOS, helping physicians make an accurate diagnosis and develop an effective treatment plan.
Ovarian cancer
Ovarian cancer is a type of cancer that originates in the ovaries, which are the female reproductive organs responsible for producing eggs. It is the fifth most common cancer among women and has the highest mortality rate among gynecological cancers.
The early stages of ovarian cancer often do not cause any noticeable symptoms, which makes it difficult to detect and diagnose. However, as the cancer progresses, symptoms such as abdominal pain, bloating, changes in bowel movements, and frequent urination may occur.
Ultrasound is a valuable tool in the diagnosis of ovarian cancer. Transvaginal ultrasound, in particular, is commonly used to visualize the ovaries and assess any abnormalities. It involves inserting a probe into the vagina to obtain detailed images of the ovaries.
During an ultrasound examination, the sonographer looks for various signs that may indicate the presence of ovarian cancer. These signs include the presence of solid masses, irregular borders, complex cysts, and the presence of blood flow within the masses. The size, location, and characteristics of any abnormalities detected are also assessed.
If ovarian cancer is suspected based on ultrasound findings, further tests such as blood tests and biopsies may be performed to confirm the diagnosis. Treatment options for ovarian cancer may include surgery, chemotherapy, and radiation therapy, depending on the stage of the cancer and the individual patient’s situation.
Ultrasound plays a crucial role in the diagnosis and management of ovarian cancer. Early detection is key to improving the prognosis and survival rates of patients with this disease. Regular screenings and awareness of the symptoms of ovarian cancer are important for early detection and timely intervention.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) refers to an infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It usually occurs as a result of a sexually transmitted infection, such as chlamydia or gonorrhea, but can also be caused by other bacteria.
Symptoms:
Women with PID may experience a variety of symptoms, including:
- Pain in the lower abdomen or pelvis
- Abnormal vaginal discharge
- Irregular menstrual bleeding
- Fever
- Painful sexual intercourse
Diagnosis:
Ultrasound imaging can play a crucial role in the diagnosis of PID. It can help identify any abnormalities in the reproductive organs, such as fluid-filled pockets or abscesses, which may be indicative of an infection. Additionally, ultrasound can help rule out other potential causes of pelvic pain, such as ovarian cysts or ectopic pregnancies.
Treatment:
Treatment for PID typically involves a combination of antibiotics to target the specific bacteria causing the infection. It is important to promptly treat PID to prevent complications, such as infertility or chronic pelvic pain. In severe cases, hospitalization may be required for intravenous antibiotic therapy.
Prevention:
Preventing PID involves practicing safe sex, using condoms, and getting tested regularly for sexually transmitted infections. It is also important to seek prompt treatment for any suspected infections to prevent their spread to the reproductive organs.
Conclusion:
Ultrasound imaging plays a vital role in the diagnosis and management of pelvic inflammatory disease. It helps identify the presence of infection and guides appropriate treatment. Early detection and treatment are essential in preventing long-term complications and promoting overall reproductive health.
Tubo-ovarian abscess
Tubo-ovarian abscess (TOA) is a severe infection in the female reproductive system that involves both the fallopian tubes and ovaries. It is typically caused by a complication of pelvic inflammatory disease (PID), which is commonly associated with sexually transmitted infections such as chlamydia and gonorrhea.
The development of a tubo-ovarian abscess occurs when the infection spreads from the cervix or vagina into the upper reproductive organs. The infection causes inflammation and the formation of pus within the fallopian tubes and ovaries, leading to the development of an abscess.
Common symptoms of tubo-ovarian abscess include severe pelvic pain, fever, vaginal discharge, and irregular menstrual bleeding. In some cases, the abscess may rupture, leading to peritonitis or sepsis, which are life-threatening conditions.
Ultrasound is an essential diagnostic tool for the evaluation of tubo-ovarian abscess. Transvaginal ultrasound is the preferred imaging modality as it provides detailed visualization of the pelvic organs. The ultrasound findings of TOA typically include a complex cystic mass with thick walls and internal debris. The abscess may also appear as a hypoechoic or anechoic fluid collection with internal septations.
In addition to ultrasound, other imaging techniques such as computed tomography (CT) or magnetic resonance imaging (MRI) may be used to further evaluate the extent of the abscess and its relationship with surrounding structures.
Treatment of tubo-ovarian abscess usually involves a combination of antibiotics and surgical intervention. Antibiotics are prescribed to control the infection, while surgery may be necessary to drain the abscess or remove any necrotic tissue. In severe cases, a hysterectomy or oophorectomy may be required.
Early diagnosis and prompt treatment of tubo-ovarian abscess are crucial to prevent complications and preserve fertility. Regular gynecological examinations, practicing safe sex, and seeking medical attention for any symptoms of pelvic infection can help reduce the risk of developing this serious condition.
Hydrosalpinx
Hydrosalpinx is a medical condition in which the fallopian tube is filled with fluid. It is usually caused by an infection, such as pelvic inflammatory disease. The presence of fluid in the fallopian tube can block the passage of the egg, leading to infertility.
Ultrasound can be used to diagnose hydrosalpinx. The fluid-filled fallopian tube can be visualized as a cystic structure on ultrasound images. The size and location of the hydrosalpinx can be assessed, and any associated complications, such as infection or torsion, can be identified.
The ultrasound findings of hydrosalpinx include a dilated and fluid-filled fallopian tube. The tube may appear as a sausage-shaped structure with thin walls. The fluid inside the tube may be anechoic or may contain debris or septations.
In addition to ultrasound, other imaging modalities such as magnetic resonance imaging (MRI) or hysterosalpingography may be used to confirm the diagnosis of hydrosalpinx. These imaging techniques can provide more detailed information about the structure and function of the fallopian tube.
Treatment options for hydrosalpinx depend on several factors, including the severity of symptoms, the desire for future fertility, and the presence of associated conditions. Conservative management, such as antibiotics or anti-inflammatory medications, may be recommended for mild cases. In more severe cases or cases where fertility is a concern, surgical intervention may be necessary to remove or repair the affected fallopian tube.
Hydrosalpinx is a condition characterized by the presence of fluid in the fallopian tube. Ultrasound is a valuable tool for diagnosing hydrosalpinx and assessing its size and location. Treatment options vary depending on the individual case, but may include conservative management or surgical intervention.
Endometriosis
Endometriosis is a condition in which the tissue that normally lines the uterus, called the endometrium, grows outside the uterus. This can cause pain, inflammation, and the formation of scar tissue. Endometriosis can affect the ovaries, fallopian tubes, bladder, and other organs in the pelvic area.
Ultrasound imaging is a valuable tool for diagnosing endometriosis. It can help identify the presence and location of endometrial implants, as well as evaluate the size and extent of lesions. Ultrasound can also be used to monitor the progression of the disease and assess the response to treatment.
During an ultrasound examination for endometriosis, a transvaginal probe is inserted into the vagina to obtain detailed images of the pelvic organs. The ultrasound waves create real-time images that can be viewed on a monitor. The imaging can reveal the presence of endometrial implants, cysts, and adhesions.
Transvaginal ultrasound is particularly useful for diagnosing deep infiltrating endometriosis, which involves the invasion of endometrial tissue into the muscles and connective tissues of the pelvis. This type of endometriosis can cause severe pain and affect fertility.
Ultrasound can also be used to guide minimally invasive procedures for the treatment of endometriosis, such as laparoscopic surgery. The images obtained during the ultrasound can help the surgeon locate and remove endometrial implants, cysts, and scar tissue.
Ultrasound is a valuable tool for diagnosing and monitoring endometriosis. It provides detailed images of the pelvic organs and can help guide treatment decisions. Early detection and treatment of endometriosis can improve outcomes and alleviate symptoms.
Ovarian endometriomas
Ovarian endometriomas, also known as chocolate cysts, are a common type of endometriosis affecting the ovaries. These cysts are filled with old blood that resembles chocolate syrup, hence the name. They occur when endometrial tissue, which normally lines the uterus, grows outside of the uterus and attaches to the ovaries.
The presence of ovarian endometriomas can cause a variety of symptoms, including pelvic pain, painful periods, and infertility. Ultrasound imaging is a valuable tool for diagnosing and monitoring ovarian endometriomas.
On ultrasound, ovarian endometriomas appear as well-defined cystic masses with thick walls. The cysts are typically filled with homogeneous, low-level echoes, representing the old blood. The size of the cysts can vary, ranging from small to large.
Color Doppler ultrasound can be used to assess the blood flow within the cysts. Ovarian endometriomas may show increased blood flow, which can be seen as vascularization within the cyst wall.
While ultrasound imaging can help in the diagnosis of ovarian endometriomas, additional tests, such as laparoscopy, may be needed to confirm the diagnosis and plan appropriate treatment.
Treatment options for ovarian endometriomas include medication to manage symptoms and surgery to remove the cysts. The choice of treatment depends on factors such as the severity of symptoms, the desire for fertility, and the size of the cysts.
Ovarian endometriomas are a common manifestation of endometriosis affecting the ovaries. Ultrasound imaging plays a crucial role in the diagnosis and management of ovarian endometriomas, providing valuable information about the size, characteristics, and blood flow of the cysts.
Deep infiltrating endometriosis
Deep infiltrating endometriosis (DIE) is a severe form of endometriosis that involves the infiltration of endometrial tissue into the surrounding organs and tissues. It is characterized by the presence of deep nodules or lesions that can invade the bowel, bladder, ureters, and other structures in the pelvis.
The diagnosis of DIE can be challenging as symptoms can vary and may mimic other conditions. However, ultrasound imaging plays a crucial role in the diagnosis and evaluation of this condition. Transvaginal ultrasound is the preferred imaging modality for evaluating the pelvis and detecting deep infiltrating endometriosis.
During the ultrasound examination, the sonographer will carefully evaluate the pelvic organs, looking for signs of endometriosis. They will look for the presence of nodules or lesions, which may appear as hypoechoic or hyperechoic areas on the ultrasound image. The size, location, and depth of the lesions will also be assessed.
In addition to the visual assessment, the sonographer may also use color Doppler imaging to evaluate the blood flow within the lesions. Increased blood flow can be a sign of active endometriosis.
Ultrasound can also help assess the involvement of nearby organs, such as the bowel or bladder. The sonographer may perform a rectal or vaginal ultrasound to evaluate the presence of endometriosis in these areas.
Overall, ultrasound imaging is an important tool in the diagnosis and evaluation of deep infiltrating endometriosis. It allows for the non-invasive assessment of the pelvic organs and can help guide treatment decisions.
Limitations in Gynecological Ultrasound Diagnosis
While gynecological ultrasound is a valuable tool in diagnosing a variety of conditions, it does have its limitations. One of the main limitations is the inability to provide a definitive diagnosis in all cases. There are certain situations where further testing or imaging may be necessary to confirm a diagnosis.
Another limitation is the dependence on the skill and experience of the sonographer performing the ultrasound. The quality of the images obtained can vary depending on the operator’s expertise, which can affect the accuracy of the diagnosis. Additionally, certain factors such as patient body habitus or the presence of bowel gas can hinder visualization and limit the information obtained from the ultrasound.
Gynecological ultrasound also has limitations in its ability to detect certain conditions. For example, small ovarian masses or early-stage endometrial cancer may be difficult to visualize on ultrasound. In these cases, additional imaging modalities or techniques may be necessary for a more accurate diagnosis.
Furthermore, gynecological ultrasound is limited in its ability to provide functional information about the reproductive organs. While it can visualize structures and detect abnormalities, it cannot assess hormonal function or evaluate the functionality of the ovaries or uterus.
It is important for healthcare providers and patients to be aware of these limitations when using gynecological ultrasound as a diagnostic tool. Understanding these limitations can help guide further testing and ensure accurate diagnosis and appropriate treatment.
Operator dependent
The accuracy of ultrasound diagnosis of gynecological diseases heavily relies on the skills and experience of the operator. The interpretation of ultrasound images requires a high level of expertise and knowledge of anatomy and pathology. A well-trained operator can identify subtle abnormalities and accurately diagnose various gynecological conditions.
However, ultrasound is highly operator dependent, meaning that the quality of the images and the accuracy of the diagnosis can vary depending on the skill level of the operator. Inexperienced operators may struggle to obtain clear and detailed images, leading to misinterpretations or missed diagnoses. It is crucial for operators to receive comprehensive training and ongoing education to improve their skills and ensure accurate diagnoses.
Operator dependency can also affect the consistency of ultrasound diagnoses. Different operators may have different interpretations of the same ultrasound image, leading to variations in diagnoses. This can be particularly challenging in cases where a second opinion or consensus is required for treatment decisions.
To minimize operator dependency, standardization of ultrasound protocols and guidelines is essential. These guidelines can help ensure that operators follow consistent imaging techniques and interpret images in a standardized manner. Regular quality control assessments and audits can also be implemented to monitor operator performance and identify areas for improvement.
Overall, while ultrasound is a valuable tool for diagnosing gynecological diseases, it is important to acknowledge the operator dependency factor. By investing in proper training, standardization, and quality control measures, we can improve the accuracy and consistency of ultrasound diagnoses in gynecology.
Not always definitive
While ultrasound imaging is a valuable tool in the diagnosis of gynecological diseases, it is important to note that it is not always definitive. There are certain limitations and challenges that can affect the accuracy of ultrasound results, leading to potential misdiagnosis or the need for further testing.
One limitation is the operator-dependent nature of ultrasound exams. The skill and experience of the sonographer can have a significant impact on the quality of the images obtained and the ability to accurately interpret them. Inexperienced or inadequately trained operators may miss subtle abnormalities or misinterpret normal structures as pathology, leading to false-positive or false-negative results.
Another challenge is the variability in pelvic anatomy and the presence of overlapping structures. This can make it difficult to differentiate between normal and abnormal findings, especially in cases where there is a lack of specific ultrasound features or when the disease is in its early stages.
In addition, certain gynecological conditions may not be well visualized or may mimic other conditions on ultrasound. For example, small ovarian cysts, endometriosis, or early-stage ovarian cancers can be challenging to detect due to their size or location. In these cases, additional imaging modalities or invasive procedures may be required for a definitive diagnosis.
It is also worth noting that ultrasound findings should always be interpreted in conjunction with the patient’s clinical history and other diagnostic tests. The combination of clinical findings, imaging results, and laboratory tests can provide a more comprehensive and accurate assessment of the gynecological condition.
Overall, while ultrasound is a valuable diagnostic tool, it is important to recognize its limitations and potential pitfalls. Close collaboration between clinicians, sonographers, and radiologists is essential to ensure proper interpretation of ultrasound findings and to guide appropriate patient management.
When Further Testing is Needed
Although ultrasound is a valuable diagnostic tool for gynecological diseases, there are cases when further testing may be required to confirm a diagnosis or provide more detailed information. Some of the situations that may warrant additional testing include:
- Complex cysts: If an ultrasound reveals a complex cyst, further testing such as a biopsy or additional imaging (such as an MRI) may be needed to determine if the cyst is benign or malignant.
- Unclear findings: In some cases, the ultrasound images may not provide a clear diagnosis. In these situations, further testing, such as a hysteroscopy or laparoscopy, may be necessary to visualize the pelvic organs directly and obtain tissue samples for analysis.
- Follow-up monitoring: If an ultrasound detects an abnormality that is not immediately concerning but may require monitoring over time, further testing may be recommended. This could include repeat ultrasounds, blood tests, or other diagnostic procedures to track changes in the condition.
- Evaluation of fertility issues: When infertility is a concern, additional testing may be required to investigate the underlying causes. This may involve specialized ultrasounds, hormone testing, or other diagnostic procedures to assess the reproductive system.
- Assessment of treatment effectiveness: If a patient is undergoing treatment for a gynecological condition, further testing may be necessary to evaluate the effectiveness of the treatment. This could involve repeat ultrasounds or other imaging studies to assess changes in the disease or condition.
While ultrasound is often sufficient for diagnosing many gynecological diseases, there are instances where further testing is needed to provide a more accurate diagnosis or gather additional information. It is important for healthcare providers to consider these situations and recommend appropriate follow-up testing when necessary.
Laparoscopy
Laparoscopy is a minimally invasive surgical procedure that allows the surgeon to examine and treat the organs inside the abdomen through small incisions in the abdominal wall. It is commonly used in gynecology to diagnose and treat various gynecological diseases.
During a laparoscopy, a laparoscope, which is a thin, lighted tube with a camera, is inserted through a small incision in the abdomen. This allows the surgeon to visualize the pelvic organs, such as the uterus, ovaries, and fallopian tubes, on a monitor. Other small incisions may be made to insert surgical instruments to perform procedures such as removing cysts, removing fibroids, or treating endometriosis.
Laparoscopy offers several advantages over traditional open surgery. It allows for a quicker recovery, less pain, and smaller scars. It also reduces the risk of complications and infection. Additionally, laparoscopy offers better visualization of the pelvic organs, allowing for more accurate diagnosis and treatment.
Common gynecological conditions that can be diagnosed and treated using laparoscopy include ovarian cysts, endometriosis, ectopic pregnancy, pelvic adhesions, and infertility issues. Laparoscopy can also be used for procedures such as tubal ligation and hysterectomy.
| Advantages of Laparoscopy | Disadvantages of Laparoscopy |
| – Quicker recovery | – Limited access to certain areas |
| – Less pain | – Requires specialized training |
| – Smaller scars | – Potential risks of complications |
| – Reduced risk of infection | – Longer operating time |
| – Better visualization | – Higher cost compared to open surgery |
Laparoscopy is a valuable tool in the diagnosis and treatment of gynecological diseases. It offers numerous advantages over traditional open surgery and allows for more accurate visualization and treatment of pelvic organs. However, it also has its limitations and potential risks, and should be performed by a skilled and experienced surgeon.
MRI
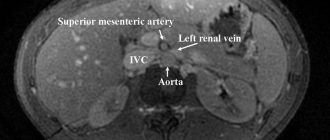
Magnetic resonance imaging (MRI) is another diagnostic tool used in the evaluation of gynecological diseases. It uses a powerful magnetic field and radio waves to generate detailed images of the pelvic region. MRI is particularly useful for assessing soft tissues and providing a more detailed view compared to ultrasound.
During an MRI scan, the patient lies on a table that slides into the MRI machine. The machine creates a magnetic field around the body, causing the hydrogen atoms in the tissues to align. When radio waves are applied, the atoms emit signals that are detected by the machine and used to construct images.
MRI can be used to evaluate various gynecological conditions, including uterine fibroids, ovarian cysts, endometriosis, and pelvic inflammatory disease. It can help determine the size, location, and characteristics of these abnormalities, aiding in diagnosis and treatment planning.
One advantage of MRI is its ability to capture images in multiple planes, allowing for better visualization and assessment of complex gynecological structures. It can also provide information about the blood flow to certain areas, which can be helpful in assessing the vascularity of tumors.
However, MRI is not without limitations. It is a more expensive and time-consuming procedure compared to ultrasound. It may also require the use of contrast agents to enhance the visibility of certain structures or abnormalities.
MRI is a valuable imaging modality for the diagnosis and evaluation of gynecological diseases. Its ability to provide detailed images of soft tissues and its multi-planar capabilities make it an important tool in the management of these conditions.
| Advantages of MRI | Limitations of MRI |
| – Detailed view of soft tissues | – Expensive |
| – Multi-planar imaging | – Time-consuming |
| – Assessment of vascularity | – Use of contrast agents |
Biopsy
A biopsy is a medical procedure in which a small sample of tissue is taken from the body for further examination. In the case of gynecological diseases, a biopsy may be performed to determine the presence of abnormal cells or to diagnose specific conditions.
There are different types of biopsies that can be performed in gynecology, depending on the suspected condition. These include:
- Colposcopy-directed biopsy: This procedure involves using a colposcope, which is a magnifying instrument, to examine the cervix. If any abnormal areas are identified, a small tissue sample is taken for analysis.
- Endometrial biopsy: This procedure involves taking a sample of the lining of the uterus (endometrium) using a thin, flexible tube. It is usually performed to investigate abnormal uterine bleeding or to evaluate the presence of endometrial cancer.
- Ovarian biopsy: In some cases, a biopsy of the ovary may be performed to examine any suspicious masses or tumors. This can help determine whether the growth is cancerous or benign.
During a biopsy, local anesthesia is usually used to numb the area being sampled. The procedure may cause some discomfort or cramping, but it is generally well-tolerated by patients. The collected tissue samples are then sent to a laboratory for analysis by a pathologist.
The results of a biopsy can provide important information about the nature of a gynecological condition, helping healthcare professionals make an accurate diagnosis and develop an appropriate treatment plan.
Question-answer:
What is ultrasound diagnosis?
Ultrasound diagnosis is a medical imaging technique that uses sound waves to produce images of the inside of the body. It is commonly used to diagnose and monitor various gynecological diseases.
How is ultrasound diagnosis performed for gynecological diseases?
Ultrasound diagnosis for gynecological diseases is typically performed by placing a transducer on the abdomen or inserting it into the vagina. The transducer emits sound waves that bounce off the organs and tissues in the pelvic area, creating images on a computer screen.
What can ultrasound diagnosis detect in gynecological diseases?
Ultrasound diagnosis can detect various gynecological diseases, including ovarian cysts, uterine fibroids, endometriosis, and polycystic ovary syndrome. It can also be used to evaluate the thickness of the uterine lining and detect abnormalities in the fallopian tubes.
Is ultrasound diagnosis painful?
No, ultrasound diagnosis is not painful. The procedure is non-invasive and does not involve any needles or incisions. Some women may experience mild discomfort during transvaginal ultrasound, but it is generally well-tolerated.
Can ultrasound diagnosis be used during pregnancy?
Yes, ultrasound diagnosis is commonly used during pregnancy to monitor the growth and development of the fetus. It can detect abnormalities in the uterus, placenta, and amniotic fluid, as well as determine the baby’s gender and estimate the due date.
What are the common gynecological diseases that can be diagnosed by ultrasound?
Ultrasound can be used to diagnose various gynecological diseases such as ovarian cysts, uterine fibroids, endometriosis, polycystic ovary syndrome (PCOS), and ectopic pregnancies.
How is ultrasound used to diagnose gynecological diseases?
During an ultrasound examination, a transducer is used to send high-frequency sound waves into the body. These sound waves bounce back and create images of the pelvic organs, allowing the doctor to evaluate the size, shape, and condition of the uterus, ovaries, and other pelvic structures. The images produced by ultrasound can help in the diagnosis of gynecological diseases.
Is ultrasound a reliable method for diagnosing gynecological diseases?
Ultrasound is considered a reliable method for diagnosing gynecological diseases. It is a non-invasive and safe procedure that provides detailed images of the pelvic organs, allowing the doctor to identify any abnormalities or diseases. However, in some cases, additional tests may be needed to confirm the diagnosis.