MALS in the Differential Diagnosis: Other Causes of Chronic Abdominal Pain
 Chronic abdominal pain is a common and often complex symptom that presents a diagnostic challenge to healthcare providers. While many cases can be attributed to gastrointestinal disorders such as irritable bowel syndrome or peptic ulcer disease, it is crucial to consider other potential causes. Among these, median arcuate ligament syndrome (MALS) has emerged as an increasingly recognized culprit, necessitating its inclusion in the differential diagnosis.
Chronic abdominal pain is a common and often complex symptom that presents a diagnostic challenge to healthcare providers. While many cases can be attributed to gastrointestinal disorders such as irritable bowel syndrome or peptic ulcer disease, it is crucial to consider other potential causes. Among these, median arcuate ligament syndrome (MALS) has emerged as an increasingly recognized culprit, necessitating its inclusion in the differential diagnosis.
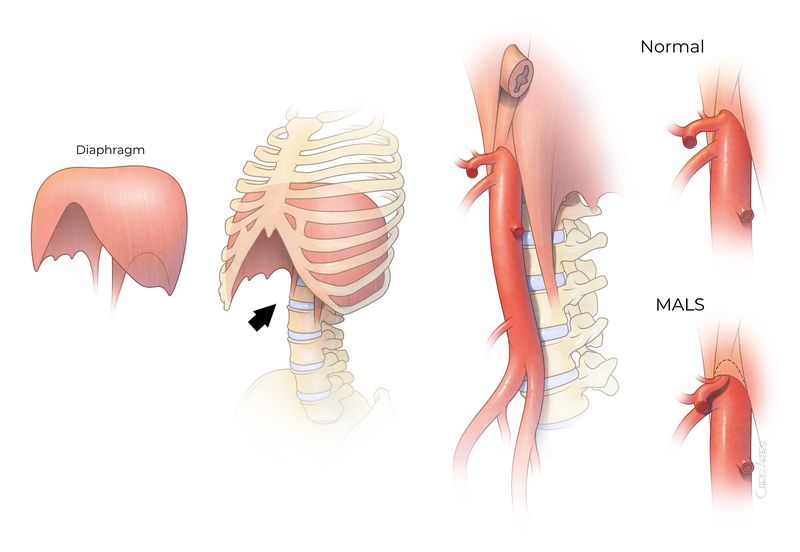
MALS is a condition characterized by the compression of the celiac artery by the median arcuate ligament, resulting in chronic abdominal pain and other associated symptoms. It can be easily overlooked due to its nonspecific clinical presentation and the absence of specific radiographic findings. However, recognizing MALS as a potential cause of chronic abdominal pain is essential in order to provide appropriate management and alleviate the patient’s symptoms.
The differential diagnosis of chronic abdominal pain should therefore encompass a comprehensive evaluation of potential etiologies, including gastrointestinal, urological, gynecological, and vascular causes. While MALS is relatively rare, its inclusion in the list of possibilities is crucial as it can significantly impact patients’ quality of life. This article aims to shed light on the importance of considering MALS in the differential diagnosis of chronic abdominal pain, highlighting its clinical features, diagnostic approaches, and management strategies.
Differential Diagnosis of Chronic Abdominal Pain
Chronic abdominal pain is a common symptom that can be caused by various conditions. A thorough differential diagnosis is essential to identify the underlying cause and guide appropriate treatment.
Some of the other causes of chronic abdominal pain include:
- Functional gastrointestinal disorders: Conditions such as irritable bowel syndrome (IBS), functional dyspepsia, and chronic constipation can present with chronic abdominal pain.
- Inflammatory bowel disease (IBD): Conditions such as Crohn’s disease and ulcerative colitis can cause chronic abdominal pain along with other symptoms like diarrhea, rectal bleeding, and weight loss.
- Gastrointestinal infections: Chronic abdominal pain can be a result of chronic infections such as Helicobacter pylori, parasitic infections, or viral infections.
- Gastroesophageal reflux disease (GERD): Chronic acid reflux can cause abdominal pain along with symptoms like heartburn and regurgitation.
- Peptic ulcer disease: Chronic abdominal pain may be caused by peptic ulcers, which are open sores in the lining of the stomach or small intestine.
- Pancreatitis: Inflammation of the pancreas can lead to chronic abdominal pain, usually accompanied by other symptoms like nausea, vomiting, and weight loss.
A comprehensive differential diagnosis also includes considering less common causes such as mesenteric artery syndrome (MALS). MALS is a rare condition characterized by compression of the celiac artery, causing chronic abdominal pain and other symptoms related to poor blood flow to the digestive organs.
In conclusion, chronic abdominal pain can have various causes, and a thorough differential diagnosis is essential to identify the underlying condition. Other common causes include functional gastrointestinal disorders, inflammatory bowel disease, gastrointestinal infections, GERD, peptic ulcer disease, and pancreatitis. Less common causes such as MALS should also be considered in the evaluation of chronic abdominal pain.
What is Chronic Abdominal Pain?
Chronic abdominal pain is a common medical condition that refers to ongoing or recurrent pain in the abdomen. It is different from acute abdominal pain, which is a sudden and severe pain that typically requires immediate medical attention. Chronic abdominal pain is characterized by persistent or intermittent pain in the abdomen that lasts for more than three months.
There are various causes of chronic abdominal pain, and it can be a challenging condition to diagnose due to the wide range of possible underlying conditions. Differential diagnosis is crucial in identifying the specific cause of the pain and developing an appropriate treatment plan.
Some of the common causes of chronic abdominal pain include:
- Gastrointestinal disorders, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or peptic ulcers
- Gallbladder problems, such as gallstones or cholecystitis
- Urinary tract disorders, such as kidney stones or urinary tract infections
- Gynecological conditions, such as endometriosis or ovarian cysts
- Musculoskeletal issues, such as muscle strains or hernias
One specific condition that can cause chronic abdominal pain is median arcuate ligament syndrome (MALS), also known as celiac artery compression syndrome. MALS occurs when the median arcuate ligament, a band of tissue in the abdomen, compresses the celiac artery, leading to reduced blood flow to the stomach and other abdominal organs. This can result in chronic abdominal pain, especially after eating.
To diagnose the specific cause of chronic abdominal pain, a detailed medical history, physical examination, and various diagnostic tests may be required. These tests may include blood tests, imaging studies (such as ultrasound, CT scan, or MRI), endoscopic procedures, or laparoscopy. A multidisciplinary approach involving gastroenterologists, urologists, gynecologists, and other specialists may be necessary to reach an accurate diagnosis.
Overall, chronic abdominal pain is a complex condition with multiple potential causes. A thorough differential diagnosis is essential in identifying the underlying condition and determining the most appropriate treatment approach.
Common Causes of Chronic Abdominal Pain
When a patient presents with chronic abdominal pain, there are several potential causes that should be considered in the differential diagnosis. These causes may include:
- Mesenteric artery compression syndrome (MALS)
- Gastrointestinal disorders, such as inflammatory bowel disease (IBD) or peptic ulcer disease
- Gallbladder disease, including gallstones or cholecystitis
- Pancreatic disorders, such as chronic pancreatitis or pancreatic cancer
- Hepatic diseases, including hepatitis or cirrhosis
- Renal conditions, such as kidney stones or urinary tract infections
- Gynecological issues, including endometriosis or ovarian cysts
- Intestinal obstruction or adhesions
- Diverticulosis or diverticulitis
- Functional disorders, such as irritable bowel syndrome (IBS) or functional dyspepsia
Each of these potential causes can present with similar symptoms, making it important for healthcare providers to conduct a thorough evaluation and diagnostic workup to determine the underlying cause of the chronic abdominal pain. MALS, in particular, is often overlooked as a possible cause of chronic abdominal pain and should be considered in patients who have not responded to initial treatment options for other potential causes.
| Cause | Symptoms | Diagnostic Tests |
| MALS | Abdominal pain, nausea, weight loss | Mesenteric duplex ultrasound, CT angiography |
| Inflammatory Bowel Disease | Diarrhea, rectal bleeding, weight loss | Colonoscopy, stool tests, blood tests |
| Gallbladder Disease | Abdominal pain, nausea, vomiting | Ultrasound, HIDA scan |
| Pancreatic Disorders | Abdominal pain, weight loss, jaundice | CT scan, MRI, blood tests |
| Hepatic Diseases | Abdominal pain, fatigue, jaundice | Liver function tests, ultrasound, biopsy |
| Renal Conditions | Flank pain, blood in urine, frequent urination | Urinalysis, ultrasound, CT scan |
| Gynecological Issues | Pelvic pain, abnormal menstrual bleeding | Pelvic exam, ultrasound, laparoscopy |
| Intestinal Obstruction | Abdominal pain, bloating, vomiting | X-ray, CT scan, physical examination |
| Diverticulosis/Diverticulitis | Abdominal pain, change in bowel habits, fever | Colonoscopy, CT scan |
| Functional Disorders | Abdominal pain, bloating, change in bowel habits | Based on symptom criteria |
By considering and evaluating for these common causes of chronic abdominal pain, healthcare providers can work towards an accurate diagnosis and develop an appropriate treatment plan for their patients.
Gastrointestinal Causes of Chronic Abdominal Pain
When evaluating the differential diagnosis of chronic abdominal pain, it is important to consider gastrointestinal causes as they are among the most common culprits. These conditions can cause ongoing pain and discomfort in the abdominal region, making it essential to identify and address them in order to provide appropriate treatment.
1. Gastroesophageal Reflux Disease (GERD): GERD is a condition in which the stomach acid flows back into the esophagus, causing irritation and inflammation. This can result in chronic abdominal pain and other symptoms such as heartburn, regurgitation, and difficulty swallowing.
2. Peptic Ulcer Disease: Peptic ulcers are open sores that develop on the lining of the stomach or the upper part of the small intestine. Chronic abdominal pain is a common symptom of peptic ulcer disease, along with other signs such as nausea, bloating, and a feeling of fullness.
3. Inflammatory Bowel Disease (IBD): IBD refers to a group of chronic conditions that cause inflammation in the digestive tract. Conditions such as Crohn’s disease and ulcerative colitis can cause ongoing abdominal pain, diarrhea, rectal bleeding, weight loss, and fatigue.
4. Irritable Bowel Syndrome (IBS): IBS is a common gastrointestinal disorder characterized by recurring abdominal pain, bloating, and changes in bowel habits. The pain is often relieved after bowel movements and is associated with other symptoms such as constipation or diarrhea.
5. Gallbladder Disease: Conditions such as gallstones or inflammation of the gallbladder can cause chronic abdominal pain, especially in the upper right quadrant. Other symptoms may include nausea, vomiting, and jaundice.
6. Pancreatitis: Pancreatitis is inflammation of the pancreas, which can lead to chronic abdominal pain. Other symptoms may include nausea, vomiting, and weight loss. Chronic pancreatitis can result in ongoing pain and digestive issues.
7. Gastrointestinal Obstruction: A blockage in the gastrointestinal tract can cause chronic abdominal pain. This can occur due to conditions such as adhesions, hernias, or tumors. Abdominal distension, vomiting, and changes in bowel movements may also be present.
8. Gastrointestinal Motility Disorders: Disorders affecting the movement of the gastrointestinal tract, such as gastroparesis or intestinal pseudo-obstruction, can cause chronic abdominal pain. These conditions disrupt the normal functioning of the digestive system and can lead to symptoms such as bloating, nausea, and changes in bowel movements.
9. Diverticulitis: Diverticulitis is inflammation or infection of small pouches that can develop in the lining of the intestine. Chronic abdominal pain, usually located in the lower left quadrant, is a common symptom of diverticulitis. Other symptoms may include fever, changes in bowel habits, and tenderness in the abdomen.
Identifying the specific gastrointestinal cause of chronic abdominal pain requires a thorough medical evaluation, including a detailed history, physical examination, and potentially additional diagnostic tests such as imaging studies or endoscopy. With an accurate diagnosis, appropriate treatment can be initiated to alleviate pain and improve the patient’s quality of life.
Non-Gastrointestinal Causes of Chronic Abdominal Pain
While mesenteric artery syndrome (MALS) is a common cause of chronic abdominal pain, there are also other non-gastrointestinal causes that should be considered in the differential diagnosis.
Chronic abdominal pain can be caused by various conditions that do not primarily involve the gastrointestinal tract. These causes may include:
- Urinary tract infections (UTIs): Infections of the urinary tract can cause pain in the lower abdomen.
- Reproductive system disorders: Conditions such as endometriosis, ovarian cysts, and pelvic inflammatory disease can cause chronic abdominal pain, especially in women.
- Renal calculi: Kidney stones can cause severe abdominal pain, often accompanied by blood in the urine.
- Neuropathic pain: Nerve-related disorders like neuropathy or nerve compression can cause chronic abdominal pain.
- Musculoskeletal disorders: Conditions such as muscle strains, hernias, or rib fractures can cause abdominal pain when the underlying muscles or bones are affected.
- Vascular disorders: Conditions like abdominal aortic aneurysm or deep vein thrombosis can cause abdominal pain due to blood vessel-related issues.
These are just a few examples of non-gastrointestinal causes of chronic abdominal pain. It is important for healthcare professionals to consider these potential causes in their differential diagnosis to ensure appropriate treatment and management of the patient’s symptoms.
When to Seek Medical Help?
If you are experiencing chronic abdominal pain, it is important to seek medical help as soon as possible. While MALS may be one cause of chronic abdominal pain, there are other potential causes that need to be considered. To help determine the cause of your pain, you should consult a healthcare professional.
A differential diagnosis is often necessary to identify the cause of chronic abdominal pain. This involves considering and ruling out other potential causes, such as gastrointestinal disorders, urinary tract infections, appendicitis, gallbladder diseases, kidney stones, pelvic inflammatory disease, and pancreatitis, among others. By seeking medical help, you can ensure that all possible causes are properly evaluated and treated.
It is important to note that MALS is a relatively rare condition, and other causes of chronic abdominal pain are much more common. However, if you have already been diagnosed with MALS or suspect that you may have it, seeking medical help is crucial for proper management and treatment.
Some signs and symptoms that may indicate the need for medical help include:
- Severe abdominal pain
- Pain that is worsening or not improving over time
- Persistent pain regardless of position or activity
- Abdominal pain accompanied by other concerning symptoms, such as fever, vomiting, or changes in bowel movements
If you experience any of these symptoms, it is important to seek immediate medical attention. Delay in diagnosis and treatment can lead to worsening of symptoms and potential complications.
Your healthcare provider will perform a thorough evaluation, which may include a physical examination, medical history review, blood tests, imaging studies, and other diagnostic tests as necessary. Based on the findings, they will be able to determine the most appropriate course of action, whether it involves further testing, referral to a specialist, or initiation of treatment.
Remember, chronic abdominal pain can have various causes, and proper diagnosis is essential for effective management and improvement of your symptoms. Do not hesitate to seek medical help if you are experiencing ongoing abdominal pain.
Diagnostic Tests for Chronic Abdominal Pain
When evaluating a patient with chronic abdominal pain, it is important to conduct a thorough differential diagnosis to identify the possible causes. Some of the tests commonly used to assess chronic abdominal pain include:
- Blood tests: These tests can help identify any abnormalities in blood cell counts, liver function, kidney function, and inflammation markers that may be contributing to the chronic abdominal pain.
- Imaging studies: Radiological imaging can provide valuable information about the structural abnormalities in the abdomen that may be causing the chronic pain. CT scans, MRI scans, and ultrasound are commonly used imaging modalities.
- Endoscopy: This procedure involves the insertion of a thin, flexible tube with a camera into the digestive tract to visualize the internal structures. Endoscopy can help identify abnormalities such as ulcers, inflammation, and tumors that may be responsible for chronic abdominal pain.
- Colonoscopy: Similar to endoscopy, colonoscopy involves the visualization of the colon and rectum using a flexible tube with a camera. This test is particularly useful in evaluating chronic abdominal pain associated with gastrointestinal disorders such as inflammatory bowel disease.
- Manometry: This test measures the pressure and motility of the gastrointestinal tract. It can help identify any abnormalities in the contractions and movements of the digestive system that may be causing chronic abdominal pain.
These are just a few examples of the diagnostic tests that may be utilized in the evaluation of chronic abdominal pain. The choice of tests may vary depending on the suspected underlying cause of the pain.
The Role of Medical Imaging
Medical imaging plays a crucial role in the differential diagnosis of chronic abdominal pain. It helps in identifying other possible causes of abdominal pain and provides valuable information for diagnosing MALS.
Medical imaging techniques such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) are commonly used to evaluate the abdominal region and identify abnormalities that may be causing chronic abdominal pain. These imaging techniques allow healthcare providers to visualize the internal structures of the abdomen and detect any signs of pathology.
Ultrasound imaging is often the first-line modality used in the evaluation of abdominal pain due to its availability, safety, and cost-effectiveness. It uses high-frequency sound waves to produce real-time images of the abdominal organs. Ultrasound can help identify conditions such as gallstones, liver or kidney abnormalities, and certain abdominal wall hernias.
CT scans are more detailed than ultrasound and provide cross-sectional images of the abdomen. They are particularly useful in identifying gastrointestinal causes of chronic abdominal pain, such as diverticulitis, inflammatory bowel disease, and tumors. CT scans can also help detect abnormalities in blood vessels, such as those seen in MALS.
MRI uses a powerful magnetic field and radio waves to generate detailed images of the abdominal organs. It can provide valuable information about the soft tissues in the abdomen, including the liver, pancreas, and spleen. MRI is often used when a more detailed evaluation is needed, or when there is concern about radiation exposure, such as in pregnant women or young patients.
In addition to these imaging techniques, there are specialized procedures such as angiography and magnetic resonance angiography (MRA) that can be used to specifically evaluate the blood vessels in the abdomen, including those supplying the mesenteric region. These procedures can help identify vascular abnormalities, such as stenosis or compression, which are characteristic of MALS.
Medical imaging plays a crucial role in the accurate diagnosis of chronic abdominal pain and distinguishing between different causes, including MALS. It allows healthcare providers to visualize and evaluate the abdominal structures and identify any abnormalities that may be contributing to the symptoms. The information provided by medical imaging helps guide further diagnostic steps and develop an appropriate management plan for patients.
Other Causes of Chronic Abdominal Pain
In the differential diagnosis of chronic abdominal pain, there are several other potential causes that should be considered alongside Median Arcuate Ligament Syndrome (MALS). These causes can range from gastrointestinal disorders to musculoskeletal issues.
- Gastrointestinal Disorders: Chronic abdominal pain can be caused by various gastrointestinal disorders such as gastroesophageal reflux disease (GERD), peptic ulcers, inflammatory bowel disease (IBD), and irritable bowel syndrome (IBS).
- Hepatobiliary Disorders: Conditions affecting the liver and biliary system, such as hepatitis, gallstones, and cholecystitis, can also present with chronic abdominal pain.
- Urinary Tract Disorders: Chronic urinary tract infections, kidney stones, and interstitial cystitis are some examples of urinary tract disorders that can cause chronic abdominal pain.
- Gynecological Conditions: Conditions specific to the female reproductive system, including endometriosis, ovarian cysts, and pelvic inflammatory disease (PID), can manifest as chronic abdominal pain.
- Musculoskeletal Issues: Chronic abdominal pain can sometimes be attributed to musculoskeletal issues, such as muscle strains, hernias, or spinal problems.
It is important for healthcare providers to consider these other potential causes and conduct a comprehensive evaluation to determine the underlying cause of chronic abdominal pain. This may involve obtaining a detailed medical history, performing a physical examination, and ordering appropriate diagnostic tests such as imaging studies, blood tests, and endoscopic procedures.
| Common Causes of Chronic Abdominal Pain | Cause |
| Gastrointestinal Disorders | Includes GERD, peptic ulcers, IBD, and IBS |
| Hepatobiliary Disorders | Conditions affecting liver and biliary system |
| Urinary Tract Disorders | Chronic UTIs, kidney stones, interstitial cystitis |
| Gynecological Conditions | Endometriosis, ovarian cysts, PID |
| Musculoskeletal Issues | Muscle strains, hernias, spinal problems |
By considering these other causes, healthcare providers can ensure comprehensive and accurate differential diagnosis of chronic abdominal pain, allowing for appropriate treatment and management strategies to be implemented.
MALS: Median Arcuate Ligament Syndrome
Median Arcuate Ligament Syndrome (MALS) is a condition that can cause chronic abdominal pain. It is characterized by the compression of the celiac artery due to the tightening of the median arcuate ligament, a fibrous band of tissue that extends from the diaphragm to the vertebral column.
MALS is considered a relatively rare condition, but it should be included in the differential diagnosis of chronic abdominal pain when other causes have been ruled out. It is particularly important to consider MALS in patients who experience postprandial pain, weight loss, and abdominal bruits.
A thorough medical history and physical examination are essential for the diagnosis of MALS. Imaging studies, such as Doppler ultrasound, computed tomography angiography (CTA), or magnetic resonance angiography (MRA), can help confirm the diagnosis by demonstrating the compression of the celiac artery.
Once MALS is diagnosed, the mainstay of treatment is surgical intervention. The most common procedure is the release of the median arcuate ligament. This can be done through an open surgery or minimally invasive techniques, such as laparoscopic or robotic-assisted surgery.
While the success rates of surgical intervention for MALS are generally high, some patients may experience recurrence of symptoms. In such cases, additional interventions, such as angioplasty or stent placement, may be necessary to relieve the compression on the celiac artery.
In conclusion, MALS is an important differential diagnosis for chronic abdominal pain. It is essential to consider this condition in patients who present with specific symptoms and findings. Prompt diagnosis and appropriate surgical intervention can provide relief and improve the quality of life for individuals with MALS.
Symptoms and Diagnosis of MALS
Median arcuate ligament syndrome (MALS) is a rare condition that can cause chronic abdominal pain. It occurs when the median arcuate ligament, a band of tissue that connects the diaphragm and the spine, presses on the celiac artery. This compression can lead to decreased blood flow to the abdominal organs, resulting in pain and other symptoms.
The symptoms of MALS can vary from person to person, but some common ones include:
- Chronic abdominal pain
- Postprandial pain (pain after eating)
- Weight loss
- Nausea and vomiting
- Abdominal bloating
- Diarrhea or constipation
These symptoms can be similar to those of other conditions, making the diagnosis of MALS challenging. A thorough medical history and physical examination are important in the differential diagnosis of chronic abdominal pain.
If MALS is suspected, further diagnostic tests may be done to confirm the diagnosis. These tests may include:
- Computed tomography (CT) scan: This imaging test can help visualize the anatomy of the abdomen and identify any compression of the celiac artery.
- Doppler ultrasound: This non-invasive test uses sound waves to assess blood flow through the celiac artery.
- Magnetic resonance angiography (MRA): This imaging test uses a magnetic field and radio waves to create detailed images of blood vessels, including the celiac artery.
- Angiography: This invasive procedure involves injecting contrast dye into the blood vessels and taking X-rays to visualize any abnormalities.
Once the diagnosis of MALS is confirmed, treatment options can be considered to alleviate the symptoms and improve blood flow to the abdominal organs. In some cases, surgical intervention may be necessary to relieve the compression on the celiac artery. It is important to consult with a healthcare professional for an accurate diagnosis and appropriate management of chronic abdominal pain.
Treatment Options for MALS
When a patient is diagnosed with Median Arcuate Ligament Syndrome (MALS), several treatment options are available to alleviate their symptoms and improve their quality of life. It’s important to note that the most effective treatment for MALS is still debated among medical professionals, and it ultimately depends on the individual case and severity of symptoms.
1. Conservative Management:
In mild cases of MALS where symptoms are not severe or debilitating, conservative management may be recommended. This approach focuses on lifestyle changes and conservative treatments to manage the symptoms.
Conservative management may involve:
- Diet modification: Avoiding trigger foods that exacerbate symptoms, such as fatty foods.
- Weight management: Maintaining a healthy weight to reduce pressure on the abdominal region.
- Physical therapy: Engaging in exercises and techniques to strengthen the abdominal muscles and improve overall function.
- Pain management: Utilizing over-the-counter pain medications to manage pain and discomfort.
2. Medications:
If conservative management does not provide sufficient relief, medications may be prescribed to help alleviate the symptoms of MALS. Some common medications that may be prescribed include:
- Antispasmodics: These medications help relax the smooth muscles of the intestine and relieve abdominal pain and cramping.
- Proton pump inhibitors (PPIs): PPIs reduce the production of stomach acid, which can help alleviate symptoms related to acid reflux and gastroesophageal reflux disease (GERD).
- Analgesics: Prescription pain medications may be used to manage more severe pain that does not respond to over-the-counter options.
3. Surgical Intervention:
In cases where conservative management and medication therapy fail to provide relief, surgical intervention may be considered. The most common surgical treatment for MALS is called median arcuate ligament release.
In this procedure, the surgeon releases the tight fibers of the median arcuate ligament to relieve the compression on the celiac artery and surrounding structures. This allows for improved blood flow to the abdominal organs and may alleviate symptoms.
It’s important to note that surgical intervention carries risks and potential complications, and should only be considered after a thorough discussion and evaluation by a medical professional.
Conclusion:
While there is no one-size-fits-all approach to the treatment of MALS, there are various options available to help alleviate symptoms and improve the quality of life for patients. Conservative management, medications, and surgical intervention are all potential avenues to explore, and the best course of treatment should be determined on a case-by-case basis in conjunction with a healthcare professional.
Q&A:
What are the common causes of chronic abdominal pain?
The most common causes of chronic abdominal pain include irritable bowel syndrome, inflammatory bowel disease, chronic pancreatitis, and peptic ulcer disease.
How is chronic abdominal pain diagnosed?
Diagnosis of chronic abdominal pain involves a thorough medical history, physical examination, and various diagnostic tests such as blood tests, imaging studies, and endoscopy.
What is MALS?
MALS stands for median arcuate ligament syndrome, which is a condition characterized by the compression of the celiac artery by the median arcuate ligament, leading to chronic abdominal pain.
What are the symptoms of MALS?
The symptoms of MALS can include chronic abdominal pain, especially after eating, weight loss, nausea, vomiting, and diarrhea.
How is MALS diagnosed?
Diagnosis of MALS involves various imaging studies such as Doppler ultrasound, computed tomography angiography, and magnetic resonance angiography to evaluate the blood flow in the celiac artery and confirm the presence of compression.