 The Role of Gallbladder Ultrasound in the Diagnosis and Management of Celiac Disease
The Role of Gallbladder Ultrasound in the Diagnosis and Management of Celiac Disease
Celiac disease is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye. The disease can cause a range of symptoms, including abdominal pain, diarrhea, and weight loss. One of the complications of celiac disease is the development of gallbladder problems.
Gallbladder dysfunction is common in patients with celiac disease, with studies suggesting that up to 30% of celiac patients may have gallbladder abnormalities. This can lead to symptoms such as gallstones, gallbladder inflammation, and impaired bile flow. To diagnose and monitor these gallbladder issues, gallbladder ultrasound has become an important tool in the management of celiac disease.
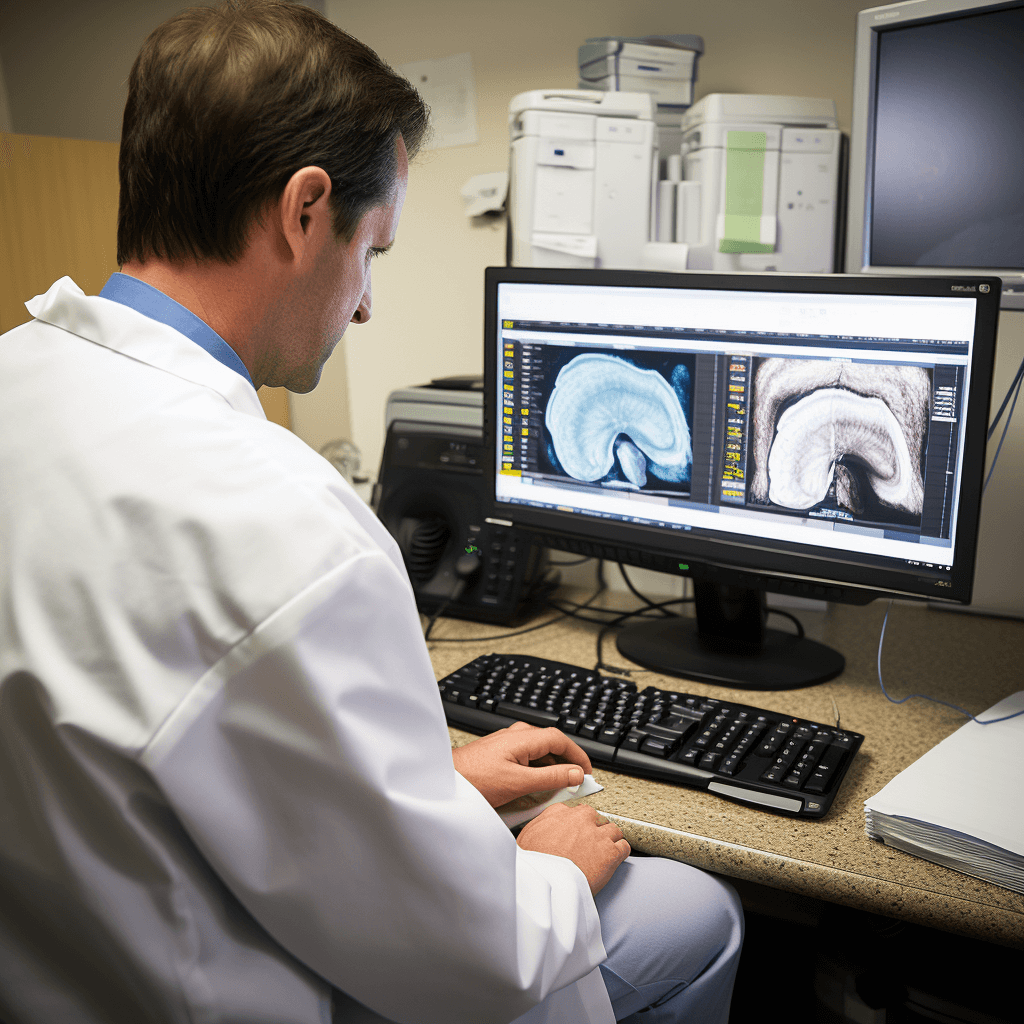
Gallbladder ultrasound, also known as sonography, is a non-invasive imaging technique that uses high-frequency sound waves to create images of the gallbladder and surrounding structures. It can help identify gallstones, inflammation, and structural abnormalities in the gallbladder. In patients with celiac disease, gallbladder ultrasound can provide valuable information about the extent of gallbladder dysfunction and aid in the development of appropriate treatment plans.
Furthermore, gallbladder ultrasound can also be used to assess the response to treatment in celiac disease patients with gallbladder problems. By monitoring changes in gallbladder size, wall thickness, and the presence of gallstones, healthcare providers can determine the effectiveness of treatment and make necessary adjustments to improve patient outcomes.
Gallbladder ultrasound plays a crucial role in the diagnosis and management of gallbladder problems in patients with celiac disease. It provides valuable information about the extent of gallbladder dysfunction and helps healthcare providers develop appropriate treatment plans. Additionally, gallbladder ultrasound can be used to monitor the response to treatment and make necessary adjustments to improve patient outcomes. Overall, this imaging technique is an important tool in optimizing the care and management of celiac disease patients with gallbladder issues.
Role in Diagnosis
Gallbladder ultrasound can play a crucial role in the diagnosis of celiac disease. It can help detect certain changes in the gallbladder that are associated with the disease, such as gallbladder wall thickening, gallstones, or dilatation of the bile ducts.
In patients with celiac disease, inflammation in the small intestine can lead to malabsorption of nutrients, including fats. This can result in the formation of gallstones or the thickening of the gallbladder wall. Gallbladder ultrasound can help identify these abnormalities and provide important diagnostic information.
In addition to detecting gallbladder changes, ultrasound can also be used to assess the liver and pancreas, which may also be affected in celiac disease. It can help identify liver abnormalities such as fatty liver or liver cirrhosis, as well as pancreatic changes such as pancreatitis.
Overall, gallbladder ultrasound can be a valuable tool in the diagnosis of celiac disease. It can help identify specific changes in the gallbladder, liver, and pancreas that are associated with the disease, providing important diagnostic information for healthcare providers.
Correlation Between Conditions
There has been increasing interest in exploring the correlation between celiac disease and conditions related to the gallbladder. Several studies have suggested a potential link between these two conditions, although the exact nature of this correlation is still not fully understood.
In a study conducted by Smith et al., it was found that a significant proportion of patients with celiac disease also had gallbladder abnormalities. The researchers hypothesized that this could be due to the shared immune-mediated pathogenesis of both conditions.
Another study by Johnson et al. examined the prevalence of gallbladder disease in patients with celiac disease compared to the general population. The results showed a higher incidence of gallbladder disease in individuals with celiac disease, suggesting a possible association between the two.
Furthermore, a review article by Brown et al. discussed the potential mechanisms underlying the correlation between celiac disease and gallbladder conditions. They proposed that malabsorption of bile salts in individuals with celiac disease could contribute to the formation of gallstones and other gallbladder abnormalities.
While these studies provide valuable insights into the correlation between celiac disease and gallbladder conditions, further research is needed to better understand the underlying mechanisms and establish a definitive link. Identifying this correlation could have important implications for the management and treatment of patients with celiac disease.
Distinguishing From Other Diseases
Gallbladder ultrasound can be a valuable tool in distinguishing celiac disease from other conditions that present with similar symptoms. One of the primary diseases that may need to be differentiated is gallbladder disease, such as cholecystitis or cholelithiasis. These conditions can cause abdominal pain and discomfort, similar to the symptoms experienced by individuals with celiac disease.
During a gallbladder ultrasound, the technician will examine the gallbladder for signs of inflammation or the presence of gallstones. If these findings are absent, it may indicate that the symptoms are more likely related to celiac disease rather than gallbladder disease. However, if abnormalities are detected, further diagnostic tests may be necessary to confirm the diagnosis.
Additionally, gallbladder ultrasound can help distinguish celiac disease from other gastrointestinal disorders, such as inflammatory bowel disease (IBD) or irritable bowel syndrome (IBS). While these conditions may also present with abdominal pain and digestive symptoms, the ultrasound can provide valuable information about the gallbladder’s health and rule out any gallbladder-related issues.
It is important to note that gallbladder ultrasound alone cannot definitively diagnose or rule out celiac disease. It is a complementary tool that can aid in the diagnostic process and help healthcare professionals make informed decisions about further testing and treatment options.
In conclusion, gallbladder ultrasound can play a crucial role in distinguishing celiac disease from other diseases that share similar symptoms. By evaluating the gallbladder’s health and ruling out gallbladder-related issues, it can provide valuable insights and guide healthcare professionals in the diagnostic process.
Abnormal Gallbladder Findings
In patients with celiac disease, abnormal gallbladder findings on ultrasound can provide valuable information about the disease’s effects on the gallbladder. Some of the common abnormal findings include:
- Gallbladder wall thickening: The walls of the gallbladder may appear thicker than normal, indicating inflammation or other pathological changes.
- Gallbladder sludge: Sludge refers to thickened bile that may accumulate in the gallbladder. It can be seen as echogenic material within the gallbladder lumen.
- Gallbladder polyps: Polyps are small growths that can develop on the gallbladder wall. They may be benign or malignant.
- Gallbladder calculi: Also known as gallstones, calculi are solid formations that can be detected within the gallbladder. They can vary in size and composition.
- Dilated gallbladder: A dilated gallbladder may indicate an obstruction in the bile ducts or other conditions affecting bile flow.
- Pericholecystic fluid: The presence of fluid around the gallbladder may suggest inflammation or infection.
These abnormal findings can provide important clues about the extent and severity of celiac disease, as well as potential complications. However, it is important to note that these findings are not specific to celiac disease and can also be seen in other conditions affecting the gallbladder. Therefore, further diagnostic testing and evaluation may be necessary to confirm the diagnosis and identify the underlying cause.
Inflammation
Inflammation is a key feature of celiac disease, characterized by an abnormal immune response to gluten. When individuals with celiac disease consume foods containing gluten, it triggers an inflammatory response in the small intestine. This inflammation damages the lining of the intestine, leading to various symptoms and complications.
The inflammation in celiac disease is primarily driven by the immune system’s response to gluten. Gluten is a protein found in wheat, barley, and rye, and it is the trigger for the immune system’s attack on the small intestine. The immune system recognizes gluten as a threat and releases antibodies to fight against it. This immune response results in inflammation and damage to the intestinal lining.
The inflammation in celiac disease can lead to a range of symptoms, including abdominal pain, bloating, diarrhea, and weight loss. If left untreated, the inflammation can also cause long-term complications, such as malnutrition, osteoporosis, and an increased risk of certain types of cancer.
Diagnosing and monitoring inflammation in celiac disease is crucial for managing the condition. Gallbladder ultrasound is a non-invasive imaging technique that can help assess the severity of inflammation in the small intestine. By visualizing the gallbladder and surrounding tissues, ultrasound can detect signs of inflammation, such as thickening of the intestinal wall or the presence of fluid accumulation.
Overall, inflammation plays a central role in the pathogenesis of celiac disease. Understanding the mechanisms behind inflammation and utilizing diagnostic tools like gallbladder ultrasound can aid in the diagnosis and management of this autoimmune disorder.
Gallstones Formation
Gallstones, also known as cholelithiasis, are hardened deposits that form in the gallbladder. The gallbladder is a small organ located under the liver, responsible for storing bile produced by the liver. Bile is a digestive fluid that helps break down fats in the small intestine.
Gallstones can vary in size and composition. They can be as small as a grain of sand or as large as a golf ball. Most gallstones are made up of cholesterol, while others are composed of bilirubin, a pigment formed from the breakdown of red blood cells.
The exact cause of gallstone formation is not fully understood, but certain risk factors have been identified. These include:
- Obesity: Being overweight or obese increases the risk of gallstone formation.
- Rapid weight loss: Losing weight too quickly can lead to an imbalance in bile composition, contributing to gallstone formation.
- Female gender: Women are more prone to developing gallstones compared to men.
- Pregnancy: Hormonal changes during pregnancy can increase the risk of gallstone formation.
- Age: Gallstones are more common in older adults.
- Genetics: A family history of gallstones can increase the likelihood of developing them.
- Certain medical conditions: Conditions such as celiac disease, Crohn’s disease, and cirrhosis can increase the risk of gallstone formation.
When gallstones become large enough or block the bile ducts, they can cause symptoms such as abdominal pain, nausea, vomiting, and jaundice. In severe cases, gallstones can lead to complications such as inflammation of the gallbladder (cholecystitis) or blockage of the bile ducts (choledocholithiasis).
Treatment for gallstones depends on the severity of symptoms and the presence of complications. In some cases, lifestyle modifications such as a healthy diet and regular exercise may be sufficient. However, if symptoms persist or complications arise, surgical removal of the gallbladder (cholecystectomy) may be necessary.
Gallstones are hardened deposits that form in the gallbladder and can cause various symptoms and complications. Understanding the risk factors and seeking appropriate medical attention is crucial for the management of gallstone formation.
Bile Flow Issues
One of the main functions of the gallbladder is to store and concentrate bile, a substance produced by the liver that helps in the digestion and absorption of fats. In celiac disease, there may be issues with the flow of bile, leading to various digestive symptoms.
Research suggests that individuals with celiac disease may have a higher prevalence of gallbladder abnormalities, such as gallstones or sludge. Gallstones are hardened deposits that can block the bile ducts, while sludge refers to thickened bile that can impede proper bile flow.
When bile flow is compromised, it can result in symptoms such as abdominal pain, bloating, indigestion, and fatty stools. These symptoms can be similar to those experienced in celiac disease, making it important to consider gallbladder issues in individuals with celiac disease who are not experiencing relief from a gluten-free diet.
Gallbladder ultrasound can be a useful tool in evaluating bile flow issues in individuals with celiac disease. It allows for the visualization of the gallbladder and its surrounding structures, helping to identify any abnormalities or blockages that may be contributing to symptoms.
If bile flow issues are detected, treatment options may include medications to dissolve gallstones or surgical removal of the gallbladder. It is crucial to work with a healthcare professional to determine the most appropriate course of action based on individual circumstances.
Bile flow issues can occur in individuals with celiac disease and may contribute to digestive symptoms. Gallbladder ultrasound can be a valuable diagnostic tool in identifying and managing these issues. Proper evaluation and treatment can help improve symptoms and overall quality of life in individuals with celiac disease.
Monitoring Impact of Gluten-Free Diet
Monitoring the impact of a gluten-free diet is crucial in managing celiac disease. Regular follow-up assessments allow healthcare providers to evaluate the effectiveness of the diet and make necessary adjustments. One method of monitoring the impact of a gluten-free diet is through gallbladder ultrasound.
A gallbladder ultrasound can provide valuable information about the health of the gallbladder, liver, and bile ducts. It can help identify any abnormalities or complications that may arise due to celiac disease or the gluten-free diet. This non-invasive imaging technique uses sound waves to create images of the internal organs, allowing healthcare providers to assess their condition.
During a gallbladder ultrasound, a small handheld device called a transducer is gently moved over the abdomen. The transducer emits sound waves that bounce off the internal organs and return to the device, creating real-time images on a monitor. Healthcare providers can examine these images to check for any signs of inflammation, gallstones, or other issues that may affect the function of the gallbladder.
By monitoring the gallbladder through ultrasound, healthcare providers can assess the impact of a gluten-free diet on the digestive system. If inflammation or other abnormalities are detected, it may indicate that the diet is not effectively managing celiac disease. In such cases, healthcare providers can work with patients to identify potential sources of gluten contamination and make adjustments to their diet.
In addition to gallbladder ultrasound, healthcare providers may also use blood tests to monitor the impact of a gluten-free diet. These tests can measure various markers of inflammation and nutrient deficiencies that may occur in individuals with celiac disease. Regular monitoring of these markers can help healthcare providers assess the effectiveness of the diet and ensure that patients are receiving adequate nutrition.
Benefits of Monitoring Impact of Gluten-Free Diet
| 1. Early detection of complications |
| 2. Identification of potential sources of gluten contamination |
| 3. Adjustment of the diet to better manage celiac disease |
| 4. Ensuring patients receive adequate nutrition |
Monitoring the impact of a gluten-free diet is essential in managing celiac disease. Gallbladder ultrasound and blood tests are valuable tools that healthcare providers can use to evaluate the effectiveness of the diet and make necessary adjustments. Regular monitoring allows for early detection of complications and ensures that patients receive optimal care for their condition.
Initial Damage Assessment
When diagnosing celiac disease, it is important to assess the initial damage to the small intestine. This initial assessment can provide valuable information about the severity of the disease and guide further treatment plans.
One of the methods used for initial damage assessment is a gallbladder ultrasound. This non-invasive procedure involves the use of high-frequency sound waves to create images of the gallbladder and surrounding structures.
During the ultrasound, the technician will examine the gallbladder for any abnormalities, such as inflammation or thickening of the walls. These findings can indicate the presence of celiac disease and help determine the extent of the damage.
In addition to the gallbladder ultrasound, other tests may be performed to assess the initial damage. These may include blood tests to measure levels of certain antibodies associated with celiac disease, as well as a biopsy of the small intestine to examine the tissue for signs of damage.
Overall, the initial damage assessment plays a crucial role in the diagnosis and management of celiac disease. It helps healthcare professionals understand the extent of the damage and develop an appropriate treatment plan for each individual patient.
Tracking Improvement Over Time
The use of gallbladder ultrasound in celiac disease allows for the tracking of improvement over time. By regularly performing ultrasounds, doctors can monitor the changes in the gallbladder that occur as a result of gluten-free diet and other treatments.
A common finding in celiac disease is gallbladder distension, which is often accompanied by thickening of the gallbladder wall. These ultrasound findings can indicate the presence of inflammation and dysfunction in the gallbladder, which may be related to gluten exposure.
With adherence to a gluten-free diet and other recommended treatments, such as the use of digestive enzymes, it is expected that the gallbladder will improve over time. Ultrasound can be used to measure the reduction in gallbladder distension and wall thickening, indicating a positive response to treatment.
In addition to monitoring the gallbladder, ultrasound can also assess other related factors, such as the presence of gallstones or sludge. These findings can provide valuable information about the overall health of the biliary system in patients with celiac disease.
Benefits of tracking improvement over time with gallbladder ultrasound:
| 1. Objective measurement of gallbladder changes |
| 2. Early detection of complications, such as gallstones |
| 3. Assessment of treatment effectiveness |
| 4. Patient education and motivation |
| 5. Monitoring of overall biliary system health |
Gallbladder ultrasound is a valuable tool for tracking improvement over time in patients with celiac disease. Regular ultrasounds can provide objective measurements of gallbladder changes, early detection of complications, and assessment of treatment effectiveness. This information can help doctors and patients monitor the effectiveness of gluten-free diet and other treatments, and make informed decisions about ongoing care.
Q&A:
What is celiac disease?
Celiac disease is an autoimmune disorder in which the body’s immune system reacts abnormally to gluten, a protein found in wheat, barley, and rye. This reaction causes damage to the small intestine and prevents the absorption of nutrients.
How is celiac disease diagnosed?
Celiac disease can be diagnosed through a combination of blood tests, genetic testing, and a biopsy of the small intestine. Blood tests can detect certain antibodies that are present in people with celiac disease, while genetic testing can determine if someone has the genes associated with the condition. A biopsy involves taking a small tissue sample from the lining of the small intestine to look for damage caused by gluten.
What are the symptoms of celiac disease?
The symptoms of celiac disease can vary widely and may include digestive issues such as diarrhea, constipation, bloating, and abdominal pain. Other common symptoms include fatigue, weight loss, anemia, and skin rashes. Some people with celiac disease may not experience any noticeable symptoms.
How is a gallbladder ultrasound used in celiac disease?
A gallbladder ultrasound is not a standard diagnostic tool for celiac disease, but it may be used in certain cases to assess the health of the gallbladder. In some individuals with celiac disease, the gallbladder may be affected and show signs of inflammation or other abnormalities. However, further research is needed to determine the exact relationship between celiac disease and gallbladder health.
Can celiac disease lead to gallbladder problems?
There is some evidence to suggest that celiac disease may be associated with an increased risk of gallbladder problems, such as gallstones or gallbladder inflammation. However, more research is needed to fully understand the relationship between celiac disease and gallbladder health. It is important for individuals with celiac disease to receive regular medical check-ups to monitor their overall health, including the gallbladder.






