Pediatric MALS: Diagnosis and Treatment Considerations for Young Patients.
Young patients with pediatric median arcuate ligament syndrome (MALS) often face unique challenges when it comes to diagnosis and treatment. MALS is a rare condition that occurs when the median arcuate ligament compresses the celiac artery, causing symptoms such as abdominal pain, digestive issues, and weight loss. These symptoms can be particularly distressing for young patients, who may struggle to communicate their symptoms effectively.
Diagnosing MALS in pediatric patients can be challenging due to the rarity of the condition and the diversity of symptoms. However, it is important for healthcare professionals to consider MALS as a potential diagnosis in young patients with unexplained abdominal pain. This requires a thorough medical history, physical examination, and further diagnostic tests such as ultrasound or computed tomography (CT) angiography.
Treatment options for pediatric MALS can vary depending on the severity of symptoms and the individual patient’s needs. In some cases, conservative management with dietary modifications and pain management may be sufficient to alleviate symptoms. However, in more severe cases, surgical intervention may be necessary to relieve the compression of the celiac artery.
When considering treatment for pediatric MALS, it is important for healthcare professionals to take into account the unique needs of young patients. This includes factors such as their growth and development, emotional well-being, and long-term prognosis. Collaborative decision-making involving the patient, their parents or guardians, and a multidisciplinary team of healthcare professionals is crucial to ensure the best possible outcome for young patients with pediatric MALS.
Pediatric MALS: Diagnosis and Treatment Considerations
When it comes to diagnosing and treating pediatric Median Arcuate Ligament Syndrome (MALS), there are several important considerations that healthcare professionals need to keep in mind. MALS is a relatively rare condition that affects young patients, and early detection and appropriate treatment are essential for managing the symptoms and preventing complications.
Diagnosis:
MALS is often challenging to diagnose in pediatric patients due to the nonspecific nature of the symptoms. Common symptoms include abdominal pain, weight loss, nausea, and vomiting. However, these symptoms can be similar to those of other gastrointestinal disorders, making it crucial to consider MALS as a potential cause.
Diagnosis of MALS typically begins with a thorough medical history and physical examination. Healthcare professionals may then order imaging tests such as Doppler ultrasound, computed tomography (CT) angiography, or magnetic resonance angiography (MRA) to visualize the celiac artery and confirm the presence of compression.
Treatment Considerations:
The optimal treatment approach for pediatric MALS depends on the severity of symptoms and the impact on the patient’s quality of life. In some cases, conservative management may be sufficient, involving dietary modifications, pain management, and close monitoring of the patient’s symptoms.
However, if conservative measures fail to provide relief or if the patient’s symptoms are severe and significantly affecting their daily life, surgical intervention may be necessary. The most common surgical procedure for MALS is called celiac artery decompression, where the ligament causing the compression is divided or removed, allowing for improved blood flow to the abdominal organs.
It is crucial to consider the patient’s age and overall health when determining the appropriate treatment course for pediatric MALS. Surgeons and other healthcare professionals should collaborate closely to ensure a comprehensive approach that addresses the patient’s specific needs and minimizes the risk of complications.
Conclusion:
Diagnosing and treating pediatric MALS requires careful consideration of the patient’s symptoms, medical history, and potential treatment options. Early detection and appropriate management can significantly improve the patient’s quality of life and prevent long-term complications. Healthcare professionals should remain vigilant and consider MALS as a potential cause when evaluating young patients with abdominal pain and other related symptoms.
Symptoms of Pediatric MALS
Pediatric MALS, or Median Arcuate Ligament Syndrome, is a rare condition that primarily affects young patients. It is important to be aware of the symptoms of Pediatric MALS in order to provide timely diagnosis and appropriate treatment.
Some common symptoms of Pediatric MALS include:
- Abdominal pain: Recurrent, severe abdominal pain is often the main symptom of Pediatric MALS. The pain is usually located in the upper abdomen, just below the ribcage.
- Weight loss: Many children with Pediatric MALS experience unintended weight loss due to reduced appetite and chronic abdominal pain.
- Nausea and vomiting: Pediatric MALS can cause symptoms like nausea and vomiting, particularly after a meal.
- Delayed gastric emptying: Some young patients with Pediatric MALS may experience delayed gastric emptying, leading to bloating and a feeling of fullness even after consuming small amounts of food.
- Postprandial pain: Children with Pediatric MALS often experience pain that worsens after eating, especially meals that are high in fat.
- Difficulties with growth and development: Pediatric MALS can affect a child’s growth and development due to inadequate nutrient absorption and chronic pain.
If a young patient presents with these symptoms, further evaluation is necessary to diagnose Pediatric MALS. The diagnosis may involve a combination of medical history, physical examination, and imaging studies, such as ultrasound or CT angiography.
It is important to consider Pediatric MALS as a potential cause of abdominal pain in young patients, particularly if other more common causes have been ruled out. Timely diagnosis and treatment can help alleviate symptoms and improve the quality of life for children with Pediatric MALS.
Early Detection and Diagnosis of Pediatric MALS
Young patients with pediatric median arcuate ligament syndrome (MALS) require early detection and accurate diagnosis to ensure appropriate treatment considerations.
Pediatric MALS refers to the compression of the celiac artery by the median arcuate ligament, resulting in symptoms such as abdominal pain and weight loss. These symptoms can be initially vague and nonspecific, making the diagnosis challenging in young patients.
The following considerations are crucial in the early detection and diagnosis of pediatric MALS:
- Clinical History: A thorough evaluation of the patient’s medical history is essential in identifying potential factors that may contribute to the development of MALS. This includes previous abdominal trauma, growth spurts, and underlying connective tissue disorders.
- Physical Examination: A comprehensive physical examination can provide valuable clues for diagnosing pediatric MALS. Abdominal tenderness, decreased bowel sounds, and arterial bruits can be indicative of celiac artery compression.
- Diagnostic Imaging: Various imaging modalities can be utilized to confirm the diagnosis of pediatric MALS. Doppler ultrasound can assess blood flow velocities in the celiac artery, while magnetic resonance angiography (MRA) and computed tomography angiography (CTA) can provide detailed anatomical information of the abdominal vasculature.
- Collaboration with Specialists: In complex cases, collaboration with specialists such as pediatric gastroenterologists and vascular surgeons is essential for an accurate diagnosis. These experts can provide additional insights based on their respective specialties.
Early detection and diagnosis of pediatric MALS is crucial to initiate appropriate treatment considerations. With prompt intervention, young patients can achieve symptom relief and improve their overall quality of life.
Imaging Techniques for Pediatric MALS Diagnosis
Diagnosing median arcuate ligament syndrome (MALS) in pediatric patients requires the use of various imaging techniques. These techniques are crucial for accurately determining the presence and severity of MALS in young patients and guiding appropriate treatment considerations.
1. Doppler Ultrasound: Doppler ultrasound is a commonly used initial screening tool for pediatric MALS diagnosis. This non-invasive imaging technique uses sound waves to evaluate blood flow through the celiac axis and can detect any abnormalities or narrowing caused by the median arcuate ligament. Doppler ultrasound is particularly useful in identifying blood flow turbulence and any significant changes in velocity.
2. Computed Tomography (CT) Angiography: CT angiography is a more advanced imaging technique that provides detailed images of the blood vessels in the abdomen. It can accurately identify the location and extent of the median arcuate ligament’s compression on the celiac artery. CT angiography helps clinicians visualize the anatomy and identify any stenosis or occlusion caused by MALS.
3. Magnetic Resonance Angiography (MRA): MRA is another imaging technique that can be used to diagnose pediatric MALS. It uses magnetic fields and radio waves to create detailed images of blood vessels. MRA provides comparable information to CT angiography but without the use of ionizing radiation, making it a safer option for young patients. However, it may not be as widely available or provide as high-resolution images as CT angiography.
4. Digital Subtraction Angiography (DSA): DSA is an invasive imaging procedure that involves the injection of a contrast dye into the bloodstream. It provides real-time X-ray images of blood flow and helps visualize any obstructions or abnormalities in the celiac artery caused by MALS. DSA is typically performed during angiography and may be reserved for cases where other imaging techniques are inconclusive.
5. Magnetic Resonance Imaging (MRI): MRI can be used as a complementary imaging technique to evaluate the surrounding structures and rule out other underlying causes of symptoms. Although it may not directly show the compression of the celiac artery, it can provide valuable information about surrounding organs and tissues.
Conclusion: Diagnosing pediatric MALS involves a combination of imaging techniques to accurately assess the presence and severity of the condition. Doppler ultrasound, CT angiography, MRA, DSA, and MRI all play important roles in guiding treatment considerations for young patients with MALS.
Laboratory Tests for Pediatric MALS Diagnosis
Diagnosing pediatric patients with Median Arcuate Ligament Syndrome (MALS) involves a comprehensive approach that includes a combination of clinical evaluations and laboratory tests. Laboratory tests can provide important insights into the patient’s overall health and can help confirm the presence of MALS.
There are several laboratory tests that can be used to aid in the diagnosis of pediatric MALS:
- Blood tests: Various blood tests can be conducted to evaluate the patient’s overall health, including complete blood count (CBC), liver function tests, kidney function tests, and pancreatic enzyme levels. These tests can help identify any abnormalities that may be associated with MALS.
- Amylase and Lipase levels: Elevated levels of amylase and lipase, enzymes produced by the pancreas, may indicate pancreatic inflammation or injury. These tests can aid in the diagnosis of MALS as pancreatic involvement is a common feature of this condition.
- Doppler ultrasound: Doppler ultrasound is a non-invasive imaging technique that uses sound waves to evaluate blood flow through blood vessels. It can be used to assess the blood flow in the celiac artery, which may be compromised in patients with MALS, leading to symptoms. Doppler ultrasound can help identify any abnormal blood flow patterns and assist in the diagnosis of MALS.
- Magnetic Resonance Angiography (MRA): MRA is an imaging test that uses magnetic fields and radio waves to create detailed images of blood vessels. It can provide a more comprehensive evaluation of the celiac artery and surrounding blood vessels, allowing for a more accurate diagnosis of MALS.
These laboratory tests, when used in conjunction with clinical evaluations and other diagnostic procedures, can help physicians diagnose pediatric patients with MALS. Early diagnosis is crucial for initiating appropriate treatment and improving outcomes for young patients with this condition.
Surgical Options for Pediatric MALS Treatment
Diagnosis and treatment of pediatric MALS (Median Arcuate Ligament Syndrome) can be challenging due to its rarity and the unique needs of young patients. While there are non-surgical treatment options available, surgery is often the most effective approach for long-term relief from MALS symptoms.
Several surgical options can be considered for the treatment of pediatric MALS, depending on the severity and specific needs of the patient:
- Laparoscopic release: This minimally invasive procedure involves cutting the median arcuate ligament to relieve the compression of the celiac artery. Laparoscopic surgery offers smaller incisions, reduced scarring, and faster recovery times compared to open surgery.
- Open surgical release: In cases where laparoscopic release is not feasible or effective, open surgical release may be performed. This involves making a larger abdominal incision to access the celiac artery and release the compression caused by the median arcuate ligament.
- Bypass grafting: In some cases, especially when the celiac artery is severely compressed or damaged, bypass grafting may be necessary. This procedure involves rerouting blood flow around the compressed area of the artery using a graft, restoring proper blood supply to the abdominal organs.
When considering surgical options for pediatric MALS treatment, it is essential to take into account the patient’s age, overall health, and specific symptoms. Collaboration between pediatric surgeons, gastroenterologists, and other specialists is crucial to ensure the best possible outcome for young patients with MALS.
Surgery is often the preferred treatment approach for pediatric MALS patients. Laparoscopic release, open surgical release, and bypass grafting are the main surgical options available, with the choice depending on the individual patient’s needs and the severity of their condition.
Non-Surgical Treatment Approaches for Pediatric MALS
When it comes to the diagnosis and treatment of pediatric median arcuate ligament syndrome (MALS), non-surgical approaches can be considered as an alternative to surgery. These approaches aim to alleviate the symptoms and improve the quality of life for pediatric patients with MALS. The decision to pursue non-surgical treatment options should be made on a case-by-case basis, taking into consideration the patient’s age, overall health, severity of symptoms, and response to conservative measures.
Here are some non-surgical treatment approaches that can be considered for pediatric MALS:
- Medication: Medications such as proton pump inhibitors (PPIs) and antacids may be prescribed to manage gastrointestinal symptoms associated with MALS, such as abdominal pain, nausea, and acid reflux. These medications help reduce the production of stomach acid and provide relief to the patient.
- Dietary modifications: Making dietary changes and avoiding trigger foods can help alleviate symptoms in some pediatric MALS patients. A healthcare professional, such as a dietitian or nutritionist, can provide guidance on appropriate dietary modifications. Common recommendations include avoiding large meals, fatty or spicy foods, and foods that may cause gas or bloating.
- Physical therapy: Physical therapy can be beneficial for pediatric MALS patients, especially those experiencing musculoskeletal symptoms such as back pain or muscle tightness. Physical therapists can develop an individualized treatment plan that includes exercises to improve posture, flexibility, and muscle strength.
- Pain management techniques: Non-surgical pain management techniques, such as acupuncture, heat therapy, or transcutaneous electrical nerve stimulation (TENS), may be utilized to alleviate pain and discomfort in pediatric MALS patients. These approaches aim to provide temporary relief and improve the patient’s overall well-being.
- Psychological support: Pediatric MALS patients and their families may benefit from psychological support to cope with the challenges associated with the condition. This can include counseling, support groups, or other mental health services to address anxiety, depression, or stress related to MALS.
It is important to note that non-surgical treatment approaches may not provide a permanent solution or cure for pediatric MALS. However, they can help manage symptoms and improve the patient’s daily functioning. Regular follow-up visits with healthcare professionals are essential to monitor the effectiveness of these approaches and make any necessary adjustments to the treatment plan.
In conclusion, non-surgical treatment approaches can be considered for pediatric MALS patients as an alternative to surgery. These approaches focus on symptom management, dietary modifications, physical therapy, pain management techniques, and psychological support. The decision to pursue non-surgical options should be made based on individual patient factors and in consultation with a healthcare professional.
Impact of Pediatric MALS on Growth and Development
Pediatric median arcuate ligament syndrome (MALS) is a rare condition that affects young patients, presenting unique considerations for diagnosis and treatment. Beyond the immediate symptoms and complications associated with MALS, this condition can also have long-term consequences on growth and development in affected children.
Growth:
- Children with MALS may experience growth delays or stunted growth due to the chronic pain, reduced appetite, and malnutrition associated with the condition.
- The inadequate blood flow to the digestive organs caused by the compression of the median arcuate ligament can impair nutrient absorption, leading to malnourishment and inadequate energy for growth.
- Height and weight percentiles may be lower than expected for age, and affected children may struggle to meet developmental milestones.
Development:
- Chronic pain and discomfort can interfere with a child’s ability to engage in normal physical activities and may affect their physical and psychosocial development.
- Children with MALS may experience fatigue and reduced energy levels, which can impact academic performance and social interactions.
- Delayed diagnosis and treatment may lead to prolonged periods of pain and physical limitations, potentially affecting self-esteem and overall psychological well-being.
Considerations:
When evaluating and treating pediatric MALS patients, healthcare providers must consider the potential impact on growth and development. Pediatric specialists, such as pediatric gastroenterologists, nutritionists, and physical therapists, may need to be involved in the comprehensive care of these patients to address specific needs related to growth and development.
Conclusion:
Pediatric MALS not only presents challenges in diagnosis and treatment but also has the potential to impact growth and development in young patients. Identifying and addressing these issues is crucial for providing comprehensive care and promoting optimal health outcomes for children with MALS.
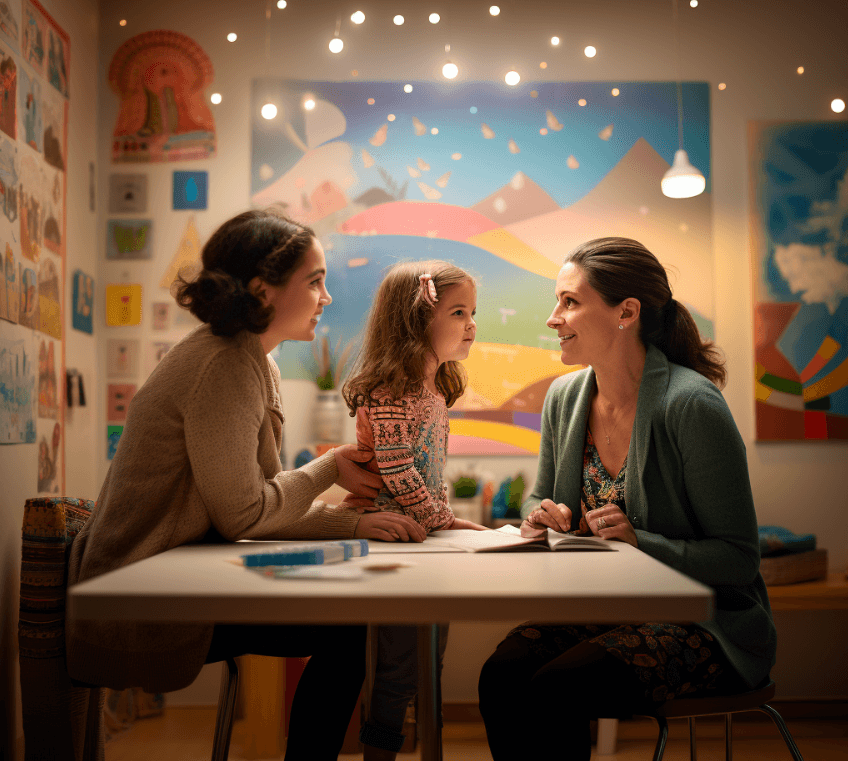
Psychological Considerations for Young Patients with Pediatric MALS
When it comes to diagnosing and treating pediatric MALS, it is important to take into consideration the psychological aspects that may affect young patients. The diagnosis of MALS in children can be a distressing experience, and understanding the psychological impact is essential for providing appropriate care and support.
A diagnosis of pediatric MALS can be overwhelming for young patients and their families. It may disrupt their daily lives and activities, leading to feelings of frustration, anxiety, and sadness. Additionally, the physical symptoms associated with MALS, such as abdominal pain, nausea, and fatigue, can further contribute to psychological distress.
Young patients with pediatric MALS may experience psychological challenges related to their self-image and self-esteem. The symptoms of MALS, such as weight loss or a distended abdomen, can affect how they perceive themselves and how others perceive them. This can lead to body image concerns and social isolation, especially during physical activities or social events.
The treatment considerations for pediatric MALS should not only focus on alleviating the physical symptoms but also on addressing the psychological well-being of young patients. Here are some important psychological considerations for young patients with pediatric MALS:
- Establishing open communication: It is crucial to create an environment where young patients feel comfortable expressing their emotions and concerns. Encouraging open communication with healthcare providers, family members, and peers can help them cope with the emotional challenges they may face.
- Providing education and information: It is essential to provide young patients and their families with clear and accurate information about MALS, its treatment options, and expected outcomes. This can help alleviate anxieties and empower them to participate in their own care.
- Offering psychological support: Young patients with pediatric MALS may benefit from psychological support services, such as counseling or therapy. These services can help them develop coping strategies, manage stress, and enhance their overall well-being.
- Encouraging social support: Engaging young patients with pediatric MALS in support groups or connecting them with peers who have similar experiences can be valuable. It provides them with a sense of belonging, understanding, and the opportunity to share their concerns and challenges.
The diagnosis and treatment of pediatric MALS require a comprehensive approach that addresses both the physical and psychological aspects of the condition. By considering the psychological well-being of young patients, healthcare providers can improve outcomes and help them navigate the challenges associated with pediatric MALS.
Dietary Modifications for Pediatric MALS Patients
Young patients with median arcuate ligament syndrome (MALS) require specific dietary modifications to manage their condition effectively. These modifications can help alleviate symptoms and improve the overall quality of life for pediatric MALS patients.
1. Limiting Fat Intake:
One of the primary dietary modifications for pediatric MALS patients is to limit their fat intake. Consuming high-fat foods can exacerbate symptoms such as abdominal pain, nausea, and vomiting. It is recommended to avoid greasy, fried, and fatty foods, including fast food, processed snacks, and fatty meats.
2. Increasing Frequency of Meals:
Instead of having three large meals per day, pediatric MALS patients may benefit from consuming smaller, more frequent meals throughout the day. This can help prevent the stomach from becoming excessively full, which can worsen symptoms. Additionally, spacing out meals can aid in better digestion and minimize discomfort.
3. Emphasizing a Balanced Diet:
A balanced diet is crucial for young patients with MALS. It is essential to include a variety of fruits, vegetables, whole grains, and lean proteins in their meals. These foods provide essential nutrients while avoiding potential triggers for symptoms. Encouraging a well-rounded diet can support overall health and aid in managing MALS symptoms.
4. Monitoring Food Triggers:
Each pediatric MALS patient may have specific food triggers that worsen their symptoms. These triggers can vary from person to person. It is important to monitor and identify any foods that may cause discomfort or flare-ups. This information can help create a personalized dietary plan that avoids these trigger foods.
5. Staying Hydrated:
Proper hydration is essential for pediatric MALS patients. Drinking an adequate amount of water throughout the day can help prevent constipation, which is a common symptom of MALS. It is important to encourage regular water intake and avoid excessive consumption of caffeinated or sugary beverages.
6. Consulting with a Registered Dietitian:
Given the unique dietary considerations for pediatric MALS patients, it is highly recommended to consult with a registered dietitian. A dietitian can provide personalized guidance and meal planning tailored to the individual needs of each patient. They can help ensure that the young MALS patient’s nutritional needs are met while minimizing symptom triggers.
In conclusion, dietary modifications play a crucial role in the management of pediatric MALS patients. By limiting fat intake, increasing meal frequency, emphasizing a balanced diet, monitoring food triggers, staying hydrated, and consulting with a registered dietitian, young MALS patients can optimize their nutrition and alleviate symptoms associated with this condition.
Recovery and Rehabilitation after Pediatric MALS Surgery
After undergoing surgical treatment for pediatric MALS, it is important for young patients to engage in a proper recovery and rehabilitation process. This will help them regain their strength, resume normal activities, and ensure long-term success of the treatment.
The recovery and rehabilitation process may vary depending on the specific case and surgical approach used. However, there are certain considerations that are generally followed:
- Pain management: Patients may experience some pain and discomfort following the surgery. Medications will be prescribed to manage pain and ensure the patient’s comfort throughout the recovery period.
- Activity restrictions: Initially, young patients will be advised to limit physical activities to allow their body to heal. The duration and intensity of the activity restrictions will depend on the individual case and the recommendation of the healthcare team.
- Dietary adjustments: Following surgery, patients may be required to make certain dietary adjustments. This can include avoiding certain foods that may trigger symptoms or adhering to a specific eating schedule. The healthcare team will provide guidance on appropriate dietary habits.
- Physical therapy: In some cases, physical therapy may be recommended as part of the rehabilitation process. This can help patients regain strength and improve mobility. Physical therapists will work closely with the patient to develop a customized therapy plan.
- Follow-up appointments: Regular follow-up appointments will be scheduled to monitor the patient’s progress and ensure that the surgical treatment was successful. These appointments will allow the healthcare team to address any concerns or complications that may arise.
The recovery and rehabilitation period after pediatric MALS surgery can vary from a few weeks to several months, depending on the individual case. It is important for young patients and their caregivers to follow the healthcare team’s instructions and participate actively in the recovery process. With proper care and adherence to the rehabilitation plan, patients can expect to return to their normal activities and enjoy improved quality of life.
Long-Term Prognosis for Pediatric MALS Patients
Diagnosis and treatment considerations for young pediatric MALS patients are crucial for ensuring their long-term prognosis.
Pediatric patients with median arcuate ligament syndrome (MALS) often experience various symptoms such as abdominal pain, postprandial symptoms, and weight loss. These symptoms can significantly impact their quality of life and daily activities.
Early diagnosis of MALS in pediatric patients is essential to start appropriate treatment promptly. Medical history, physical examination, and imaging studies like Doppler ultrasound, computed tomography (CT), and magnetic resonance angiography (MRA) play a vital role in diagnosing MALS in young patients.
Once the diagnosis is confirmed, treatment options need to be evaluated. Conservative management may include dietary modifications, pain management, and physical therapy. However, in cases where symptoms persist or worsen, surgical intervention may be necessary.
The long-term prognosis for pediatric MALS patients can vary depending on various factors. Early diagnosis and appropriate treatment can lead to symptom improvement and an improved quality of life. However, some patients may continue to experience symptoms despite treatment.
Regular follow-up visits are important to monitor the progress of pediatric MALS patients. Close monitoring can help detect any recurrence of symptoms or the development of new complications.
It’s important to note that pediatric MALS patients may require ongoing medical management even after surgical intervention. Regular check-ups with a healthcare provider can ensure that any potential issues are addressed promptly.
In conclusion, successful management of pediatric MALS patients requires a multidisciplinary approach involving healthcare providers, surgeons, and patients’ families. Early diagnosis, appropriate treatment, and regular follow-up visits can greatly contribute to the long-term prognosis and overall well-being of young patients with MALS.
Supportive Care for Pediatric MALS Patients and their Families
Diagnosing and treating pediatric MALS requires special considerations due to the young age of the patients. In addition to medical intervention, supportive care plays a crucial role in enhancing the overall well-being of both the pediatric MALS patients and their families.
1. Education and Communication:
Providing comprehensive education about pediatric MALS to patients and their families is essential for better management. This includes explaining the diagnosis, treatment options, potential complications, and the long-term prognosis. Effective communication between the healthcare team, patients, and families helps in building trust and facilitates shared decision-making.
2. Emotional Support:
Being diagnosed with a chronic condition like MALS can be emotionally challenging for young patients and their families. Psychological counseling and support groups can help them cope with anxiety, fear, and other emotional issues related to the condition. Encouraging open discussions about their feelings and concerns can promote mental well-being and a sense of belonging.
3. Nutritional Support:
Pediatric MALS patients often struggle with poor appetite, weight loss, and malnutrition due to the compression of the celiac artery. Nutritional support from a registered dietitian is essential to address these challenges and ensure proper growth and development. A well-balanced diet tailored to the individual needs of the patient can help optimize nutrition and energy levels.
4. Physical Therapy:
Physical therapy can play a vital role in improving the overall physical function and quality of life of pediatric MALS patients. A specialized physical therapy program can help alleviate pain, improve mobility, and enhance muscle strength. It is important to establish a tailored exercise regimen in collaboration with healthcare professionals to prevent muscle deconditioning.
5. Care Coordination:
Coordinating care among different healthcare providers involved in the management of pediatric MALS is crucial for optimal outcomes. This includes regular follow-up appointments, ensuring appropriate testing, and coordinating consultations with specialists as needed. Care coordination also involves facilitating communication between the primary care provider, surgeon, radiologist, and other healthcare team members.
6. Financial Support:
Pediatric MALS treatment and management can pose a financial burden on the families. Providing information about available financial resources, such as insurance coverage, community programs, and support organizations, can help alleviate financial stress. Social workers can assist families in navigating financial challenges and accessing necessary resources.
7. Peer Support:
Connecting pediatric MALS patients and their families with others who are going through similar experiences can provide valuable support and encouragement. Peer support groups, both in-person and online, can serve as a platform for sharing experiences, exchanging information, and finding emotional reassurance.
Overall, a multidisciplinary approach that addresses the physical, emotional, and practical needs of pediatric MALS patients and their families is crucial for comprehensive supportive care. By providing comprehensive support, healthcare professionals can help improve the overall quality of life for these patients and promote their long-term well-being.
Educational Considerations for Young Patients with Pediatric MALS
When it comes to the diagnosis and treatment of pediatric median arcuate ligament syndrome (MALS), it’s important to consider the unique needs of young patients. In addition to medical interventions, educational considerations play a crucial role in ensuring the well-being and success of these individuals.
1. Early diagnosis: Detecting pediatric MALS at an early stage is vital in order to provide appropriate treatment and support. It’s essential for healthcare professionals, educators, and parents to be aware of the signs and symptoms of this condition in order to facilitate timely diagnosis.
2. School accommodations: Young patients with pediatric MALS may experience various physical and cognitive symptoms that can impact their ability to participate fully in school activities. It’s important for educational institutions to implement necessary accommodations, such as providing extra breaks, modified physical education activities, and individualized education plans, to support these students
3. Communication with educators: Regular communication between healthcare providers, parents, and educators is essential in order to ensure that the educational needs of young patients with pediatric MALS are met. This collaboration allows for the exchange of important information and the development of strategies to support the academic success of these individuals.
4. Emotional support: The diagnosis of pediatric MALS can be overwhelming for both the patient and their families. Schools should provide emotional support services, such as counseling or support groups, to help young patients cope with the challenges they may face in their educational journey.
5. Flexibility: Due to the unpredictable nature of pediatric MALS symptoms, it’s important for education institutions to be flexible in their approach. This may include providing options for remote learning or accommodating missed school days for medical appointments or procedures.
6. Peer education: Educating peers about pediatric MALS can help create a supportive and inclusive environment for young patients. Schools can support peer education initiatives by providing resources and information to students, encouraging empathy, and promoting awareness of this condition.
7. Ongoing monitoring and evaluation: Regular monitoring and evaluation of a young patient’s educational progress is crucial. This allows healthcare providers, parents, and educators to assess the effectiveness of interventions and make necessary adjustments to support the educational needs of the patient.
In conclusion, the treatment and diagnosis of pediatric MALS require careful consideration of the educational needs of young patients. By implementing appropriate educational accommodations, promoting communication, and providing emotional support, healthcare providers and educators can help these individuals succeed academically and emotionally.
Research Advances in Pediatric MALS Diagnosis and Treatment
Considerations for the diagnosis and treatment of pediatric MALS hold a significant importance, as young patients require specific attention and care. The condition of median arcuate ligament syndrome (MALS) in children has been an area of active research, with several advances providing valuable insights for healthcare professionals.
Diagnosis:
- Improved Imaging Techniques: Advances in imaging technologies, such as CT angiography and magnetic resonance angiography, have greatly enhanced the diagnosis of pediatric MALS. These non-invasive techniques provide detailed images of the abdominal region, allowing physicians to accurately identify the compression of the celiac artery by the median arcuate ligament.
- Diagnostic Criteria: Researchers have developed specific diagnostic criteria for pediatric MALS, considering the unique characteristics of young patients. These criteria take into account factors such as age, symptoms, and imaging findings to guide the diagnosis process and improve accuracy.
Treatment:
- Minimally Invasive Procedures: Research has shown promising results with minimally invasive treatment options for pediatric MALS, such as laparoscopic median arcuate ligament release. These procedures offer a less invasive approach, allowing for quicker recovery and reduced post-operative complications in young patients.
- Multidisciplinary Approach: The management of pediatric MALS often requires a multidisciplinary team, including pediatric surgeons, gastroenterologists, and anesthesiologists. Research has emphasized the importance of collaborative care to ensure comprehensive evaluation, decision-making, and post-treatment follow-up for young patients.
- Long-Term Outcomes: Recent studies have focused on evaluating the long-term outcomes of pediatric MALS treatment. This research aims to determine the effectiveness and durability of different treatment approaches, providing important insights for the management of young patients with this condition.
Overall, the research advances in pediatric MALS diagnosis and treatment have significantly contributed to improving patient care for young individuals. The development of specific diagnostic criteria, advancements in imaging techniques, and the exploration of minimally invasive procedures demonstrate the dedication of researchers in optimizing outcomes for pediatric MALS patients.
Case Studies of Pediatric MALS in Young Patients
Pediatric median arcuate ligament syndrome (MALS) is a rare condition that affects young patients. MALS occurs when the median arcuate ligament, a fibrous band of tissue that attaches the diaphragm to the spine, compresses the celiac artery. This compression can lead to symptoms such as abdominal pain, weight loss, and difficulty eating.
Diagnosing pediatric MALS requires a thorough medical history, physical examination, and imaging studies. Young patients often present with nonspecific symptoms, making diagnosis challenging. However, common diagnostic tests include Doppler ultrasound, computed tomography angiography (CTA), and magnetic resonance angiography (MRA).
Treatment considerations for young patients with MALS involve a multidisciplinary approach. The goal is to alleviate symptoms and improve quality of life. In some cases, conservative measures such as dietary changes and pain management may be sufficient. However, surgical intervention may be necessary for patients with severe symptoms or complications.
Here are two case studies of pediatric MALS in young patients:
- Case 1: A 12-year-old girl presented with chronic abdominal pain, nausea, and weight loss. After a thorough evaluation, including imaging studies, she was diagnosed with MALS. Conservative measures, such as dietary modifications and pain medication, provided some relief, but her symptoms persisted. Eventually, she underwent laparoscopic median arcuate ligament release, which led to significant improvement in her symptoms.
- Case 2: A 16-year-old boy complained of postprandial abdominal pain and weight loss. Diagnostic tests revealed compression of the celiac artery consistent with MALS. Conservative management, including dietary changes and pain medication, was initially attempted but did not provide long-term relief. The patient eventually underwent open surgical release of the median arcuate ligament, which resulted in a resolution of his symptoms.
These case studies demonstrate the variability in the presentation and management of pediatric MALS. Each patient requires an individualized approach to diagnosis and treatment. The involvement of a multidisciplinary team, including pediatric gastroenterologists, surgeons, and radiologists, is crucial in ensuring the best outcomes for these young patients.
Preventive Measures and Lifestyle Changes for Pediatric MALS
When it comes to pediatric median arcuate ligament syndrome (MALS), there are several preventive measures and lifestyle changes that can be considered to manage the condition. These measures aim to alleviate symptoms and improve the overall quality of life for young patients.
- Dietary modifications: It is important for pediatric MALS patients to follow a balanced and nutritious diet. This may include incorporating more fruits, vegetables, whole grains, and lean proteins into their meals. Avoiding trigger foods that can exacerbate symptoms, such as fatty and spicy foods, may also be beneficial.
- Regular exercise: Engaging in regular physical activity can help improve blood flow and strengthen abdominal muscles. Low-impact exercises, such as walking, swimming, and yoga, are often recommended for young patients with MALS.
- Stress management: Stress can worsen symptoms of MALS in pediatric patients. Implementing stress management techniques, such as deep breathing exercises, meditation, and engaging in hobbies or activities that promote relaxation, can be beneficial in reducing stress levels.
- Proper posture: Encouraging good posture is essential for pediatric MALS patients. Sitting and standing up straight can help relieve pressure on the abdomen and improve blood flow.
- Weight management: Maintaining a healthy weight is crucial for pediatric MALS patients. Excess weight can put additional strain on the abdomen, potentially worsening symptoms. Working with a healthcare professional to develop a weight management plan may be beneficial.
In addition to these preventive measures and lifestyle changes, it is important for young patients with MALS to receive appropriate medical care. This may include regular check-ups, monitoring of symptoms, and discussions about potential treatment options.
Summary of Preventive Measures and Lifestyle Changes for Pediatric MALS:
| Measure | Description |
| Dietary modifications | Incorporate balanced and nutritious foods, and avoid trigger foods. |
| Regular exercise | Engage in low-impact exercises to improve blood flow and strengthen abdominal muscles. |
| Stress management | Implement stress reduction techniques to alleviate symptoms exacerbated by stress. |
| Proper posture | Encourage good posture to relieve pressure on the abdomen. |
| Weight management | Maintain a healthy weight to reduce strain on the abdomen. |
By incorporating these preventive measures and lifestyle changes, pediatric MALS patients can better manage their condition and improve their overall well-being.
Pediatric MALS in Adolescents: Unique Challenges and Considerations
Diagnosing and treating median arcuate ligament syndrome (MALS) in adolescents presents unique challenges due to the young age of the patients and their specific needs. MALS is a rare disorder characterized by compression of the celiac artery by the median arcuate ligament, leading to symptoms such as abdominal pain and weight loss.
In young patients, the diagnosis of MALS can be challenging as the symptoms may be nonspecific and overlap with other common conditions. Careful consideration should be given to the patient’s medical history, physical examination findings, and imaging studies to make an accurate diagnosis. It is important to rule out other possible causes of abdominal pain in adolescents, such as gastrointestinal disorders or musculoskeletal conditions.
Once the diagnosis of MALS is confirmed, treatment options should be carefully considered in the context of the patient’s age and overall health. The goal of treatment is to relieve the compression of the celiac artery and alleviate symptoms. In adolescents, conservative management with dietary modifications and physical therapy may be considered as the first line of treatment, especially if the symptoms are mild and do not significantly interfere with daily activities.
However, in cases where conservative management fails to provide relief or the symptoms worsen, surgical intervention may be necessary. Surgical options include laparoscopic median arcuate ligament release or open surgical decompression. The choice of surgical technique should take into account the patient’s age, anatomical factors, and the surgeon’s expertise.
Postoperative care and follow-up for adolescents with MALS should also be tailored to their specific needs. Close monitoring of symptoms and regular follow-up visits are essential to ensure the success of the treatment and to address any complications or recurrence of symptoms. Multidisciplinary care involving pediatric surgeons, gastroenterologists, and nutritionists may be beneficial in providing comprehensive care for these young patients.
In conclusion, pediatric MALS in adolescents presents unique challenges in terms of diagnosis and treatment. Careful consideration of the patient’s age, symptoms, and overall health is crucial in order to provide appropriate and effective management. Collaboration between healthcare providers and an individualized approach to treatment can optimize outcomes for these young patients.
Collaborative Approaches to Pediatric MALS Management
When it comes to the diagnosis and treatment of pediatric median arcuate ligament syndrome (MALS), a collaborative approach involving a multidisciplinary team of healthcare professionals is essential. This ensures that the unique needs of young patients are met and that the most appropriate treatment plan is chosen.
Some important considerations in the management of pediatric MALS include:
- Accurate diagnosis: Pediatric MALS can present with a variety of symptoms that may overlap with other conditions. Therefore, it is crucial to have a team of specialists, including pediatric surgeons, gastroenterologists, and radiologists, who are experienced in diagnosing MALS in young patients.
- Comprehensive evaluation: A thorough evaluation of the patient’s medical history, symptoms, and physical examination is essential to determine if MALS is the underlying cause. This may involve imaging studies such as computed tomography angiography (CTA) or magnetic resonance angiography (MRA) to visualize the celiac artery compression.
- Individualized treatment plan: The treatment plan for pediatric MALS should be tailored to the unique needs of each patient. This may include conservative measures such as dietary modifications and pain management, as well as surgical intervention if conservative measures are ineffective in relieving symptoms.
- Long-term follow-up: Pediatric patients with MALS require long-term follow-up to monitor their symptoms and adjust their treatment plan if necessary. Regular communication between the healthcare team and the patient’s primary care provider is crucial in ensuring optimal management of the condition.
A collaborative approach to pediatric MALS management not only improves the accuracy of diagnosis and treatment but also ensures that the emotional and psychological needs of young patients are addressed. By working together, healthcare professionals can provide the best possible care for children with MALS and help them lead healthy and fulfilling lives.
Question-answer:
What is pediatric MALS?
Pediatric MALS, also known as Median Arcuate Ligament Syndrome, is a rare condition in which the median arcuate ligament, a structure in the abdomen, presses on the celiac artery causing symptoms of abdominal pain and difficulty eating.
How is pediatric MALS diagnosed?
Pediatric MALS is diagnosed through a combination of medical history, physical examination, imaging tests such as Doppler ultrasound, computed tomography angiography (CTA), and magnetic resonance angiography (MRA), and sometimes a celiac artery compression test.
What are the treatment options for pediatric MALS?
Treatment options for pediatric MALS include conservative management with dietary changes, medication for pain relief, and regular monitoring, as well as surgical intervention in severe cases. The surgical treatment involves releasing the median arcuate ligament and restoring normal blood flow in the celiac artery.
Is pediatric MALS a lifelong condition?
Pediatric MALS can be a lifelong condition if left untreated, but with appropriate management and treatment, many patients experience significant improvement or complete resolution of their symptoms.