Pseudo Nutcracker Syndrome: Myths, Realities, and Overlaps.
When it comes to nutcracker syndrome, many misconceptions and myths circulate, leading to confusion and misunderstandings. In this article, we will debunk these myths, shed light on the realities of this condition, and explore its potential overlaps with other disorders.
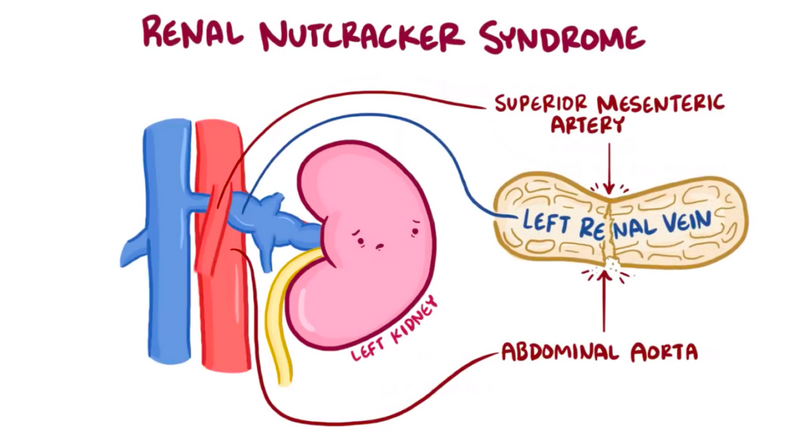
Firstly, it is important to clarify that nutcracker syndrome is a real medical condition, despite the term “nutcracker” sounding rather peculiar. It refers to the compression of the left renal vein between the abdominal aorta and the superior mesenteric artery. This compression can result in various symptoms, such as hematuria, pelvic congestion, and flank pain.
However, there is a related condition called pseudo nutcracker syndrome, which often leads to confusion. Pseudo nutcracker syndrome is not a true compression of the left renal vein but rather a result of other anatomical or physiological factors, such as abnormal renal mobility or vascular variants. In contrast, median arcuate ligament syndrome presents a different set of challenges and Mals Syndrome Symptoms. It is essential to distinguish between these conditions to ensure proper diagnosis and treatment.
Moreover, understanding the realities of nutcracker syndrome and pseudo nutcracker syndrome can facilitate the identification of potential overlaps with other disorders. For instance, some patients with nutcracker syndrome may also exhibit symptoms of pelvic congestion syndrome or may have underlying connective tissue disorders. Recognizing these overlaps can help healthcare professionals provide comprehensive and personalized care to individuals with these complex conditions.
Debunking the myths surrounding nutcracker syndrome and understanding the realities of this condition are crucial for accurate diagnosis and appropriate management. By differentiating between nutcracker syndrome and pseudo nutcracker syndrome, and exploring potential overlaps with other disorders, we can improve the quality of care and outcomes for individuals affected by these conditions.






